Although cancers are often multifactorial in origin, it is now widely understood that these trends are at least partly driven by environmental exposures. While the incidence of various kinds of cancer across the entire US population has varied in recent years, the increase among younger people is particularly concerning.
Childhood acute lymphoblastic leukemia (ALL) is another example of a cancer on the rise. For decades, the incidence of ALL has been increasing in the US, and is now the most common type of cancer in children. While advances in medicine have led to increased survival rates, survivors of ALL face a range of health and wellness difficulties later in life.12
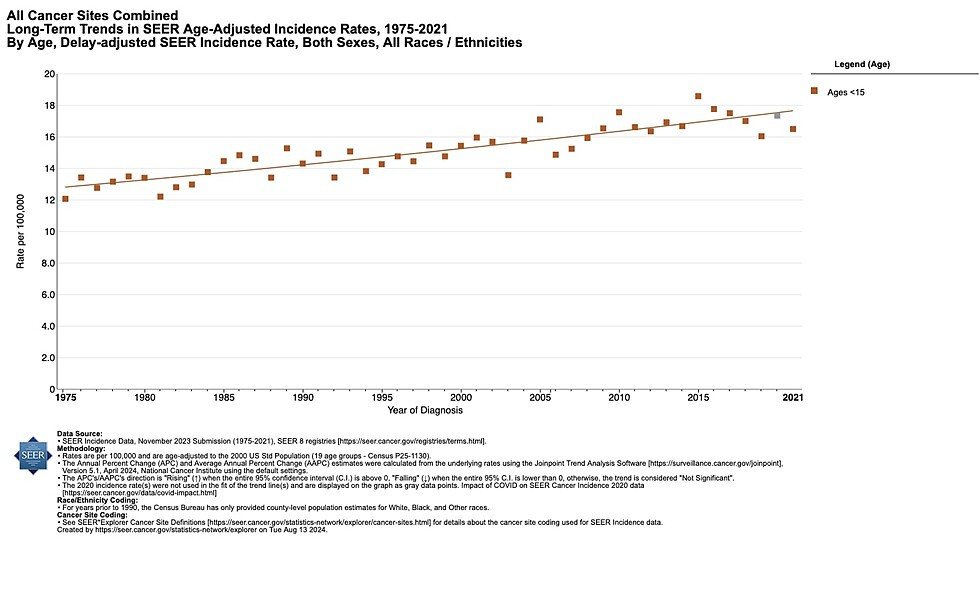
Other childhood cancers are also increasing. The graph below shows the steadily rising incidence rate of childhood cancer in the US since 1975.3 In the US, cancer is the leading cause of disease-related death past infancy among children. Evidence that environmental contaminants are driving these increases in cancer continues to grow.
Vulnerable Populations
Systemically marginalized communities often bear a disproportionate burden from environmental exposures and harms. For example, polluting industries that emit large quantities of carcinogens (such as refineries, coal-fired power plants, and plastic production facilities) are often located near low-income communities and communities of color. These “fenceline communities” often experience elevated cancer rates. (link to landing page)
Children are exposed to carcinogenic chemicals through every route of exposure (air, water, food, and skin contact) and in the many environments they experience daily (school, home, cars). They are at increased risk for several reasons:
- Because children are smaller and known to intake more air and water for body size versus adults, they receive a proportionately higher level of exposure than adults.
- Some of the metabolic pathways that provide detoxification in the body are not fully developed in the first few years of life, potentially amplifying any negative effects of exposure.
- Cancerous changes that start in childhood have an entire lifetime to manifest and propagate in the body. Thus the younger a person is when exposed, the more opportunity there is throughout the lifespan for cancer to develop. This is especially concerning given the increasing use of CT scans and nuclear medicine for diagnosis and treatment of childhood illness.5
In addition, during fetal development and infancy, the growing child’s body is constantly adapting to specific environmental conditions while cells are rapidly dividing as organs and physiologic systems develop. The epigenome, which controls gene expression, is especially vulnerable to environmental exposures and toxicants during these developmental stages. Exposures during these vulnerable windows can increase the risk of cancer later in life.
Women frequently carry a larger body burden of endocrine disrupting chemicals than men, placing them and their developing children at a higher risk of cancers related to hormone disruption.6 Those living in countries with a low Human Development Index (HDI) bear an inequitable cancer burden. For example, in countries with a very high HDI, 1 in 12 women will be diagnosed with breast cancer in their lifetime and 1 in 71 women die of it. In contrast, in countries with a low HDI, only 1 in 27 will be diagnosed but 1 in 48 women will die from it.7
“Women in lower HDI countries are 50% less likely to be diagnosed with breast cancer than women in high HDI countries, yet they are at a much higher risk of dying of the disease due to late diagnosis and inadequate access to quality treatment.”8
Workers in occupations with higher exposures to environmental cancer-causing agents are at higher risk of cancer. These include jobs in mining, manufacturing, fire fighting, construction, agriculture, and certain service industries. These jobs are often held by people from disadvantaged populations, making environmentally caused cancer outcomes an issue of health equity and environmental justice.9
The Biology of Cancer
A wide range of chemical and physical agents, both natural and human-generated, may cause cancer. The primary focus of our work at CHE is on chemical and other toxicant contributors to cancer. In this section, we discuss how the environment can interact with our bodies to cause cancer. In the next section, we go into more detail on environmental exposures linked to cancer risk.
The connections between specific toxicants and specific cancers are not always clear. Cancer is a disease of aberrant cells. Cancer cells form in response to the environment within and around them. It takes a number of steps for a healthy cell to become cancerous. Identifying exactly which single or combination of environmental factors pushes cells along which of these steps toward cancer is complex. Risk factors act within multidimensional causal webs. These risk factors include diet, lifestyle factors, and chemical exposures. As a report from the Toxics Use Reduction Institute (TURI) explains:
“Some researchers have used the metaphor of a pie to describe the factors involved in the causal mechanism of an individual’s cancer. Each slice of the pie is a component cause contributing to the development of cancer. A given causal mechanism of cancer therefore requires the joint action of many component causes. One slice could represent an inherited genetic trait; another slice could represent a lifestyle risk factor, such as smoking; another slice could represent an occupational exposure to one or more carcinogens; and so on. By removing any one of those slices of the pie, the causal mechanism cannot be completed and cancer is prevented.”10
In addition, the risks for cancer result from the complex interactions between these environmental exposures and gene variants. Some gene variants can be beneficial, providing protection against the harmful effects of outside agents, while other gene variants can make a person more susceptible. Other factors, such as the timing of exposure, can also affect cancer risk later in life.
An example of the complexity of showing a definitive connection between a toxicant and cancer is with Endocrine-Disrupting Chemicals (EDCs) and breast cancer. Research shows that exposure to some EDCs in puberty increases the risk of breast cancer occurring during a person’s lifetime.11 While it might not be possible to link a specific case of breast cancer to EDC exposure, over time and at the population level, more EDCs in the environment will likely lead to an increase in the incidence of breast cancer. Even without a full understanding of the impacts of specific toxicants, we can still take precautionary steps to protect human health.
Genetics and Cancer
Genetic makeup can increase the likelihood that certain cancers will develop. For example, about 13 percent of American women will develop breast cancer sometime during their lives, but the most recent estimates are that 55 to 72 percent of women who inherit a harmful BRCA1 mutation and around 45 to 69 percent of women who inherit a harmful BRCA2 mutation will develop breast cancer by age 70–80.12 Genomic science is helping to explain why some people are more susceptible to cancer than others. However, cancers resulting from single genes inherited from parents comprise fewer than five percent of all cancers in the US.13 Environmental insult is clearly involved in many—perhaps most—cancers.
Healthy gene expression is critical to normal cellular processes including cell growth and normal cell death. Environmental contaminants can interfere with normal biological processes by changing the chemical tags on DNA that regulate gene expression. This is known as epigenetic modification. Through changes in the epigenetic marks on cancer-related or cellular cycle genes, genes that suppress tumor growth or facilitate programmed cell death may be silenced, while genes that promote cellular growth may be overexpressed.14
Environmental toxicants can also affect cellular migration during fetal development, as was the case with diethylstilbestrol (DES). This drug was prescribed to thousands of pregnant women between 1938 and 1971 for the prevention of miscarriages. We now know that endocrine disrupting, genotoxic, and epigenetic effects of this drug inhibit the proper development of the reproductive tract in the developing fetus, especially in females, and increases the risk of rare types of vaginal and cervical cancer in daughters. Daughters are also at increased risk of breast cancer.15 There are some data to suggest these epigenetic effects could also be inherited by the granddaughters of the original DES patients.16
Characteristics of Chemical Carcinogens
DNA damage or replication mistakes occur regularly in normal cells for various reasons, including interaction with chemicals produced in cells and after exposure to toxic chemicals from outside sources. A robust repair mechanism rapidly fixes DNA damage most of the time. However, if the DNA is repaired incorrectly, a mutation can be established and persist.
Many mutations have no effect, some have minor effects, and a small number have life-threatening effects. Some mutations cause a cell to divide uncontrollably, becoming a malignant cell and causing cancer. Chemicals that induce mutations in DNA are called mutagens, and when these changes lead to cancer, the chemical is called a carcinogen.
Carcinogens can contribute to cancer through additional mechanisms to transform healthy cells toward overt cancer. The International Agency for Research on Cancer (IARC) of the World Health Organization convened a group of experts in 2016 that identified ten key characteristics, one or more of which are commonly exhibited by established human carcinogens. The ten characteristics are the abilities of a chemical agent to:
- act as an electrophile either directly or after metabolic activation (an electrophile is a chemical that readily forms bonds with certain other chemicals)
- be genotoxic (cause chromosome damage/mutations)
- alter DNA repair or cause genomic instability
- induce epigenetic alterations (alter gene expression)
- induce oxidative stress (which can lead to mutations)
- induce chronic inflammation
- suppress the immune system
- modulate receptor-mediated effects (like endocrine disruption)
- cause immortalization (interfere with normal programmed cell death)
- alter cell proliferation, cell death, or nutrient supply17
Combined and Interacting Effects
Chemical mixtures or exposure to multiple agents can increase the incidence of cancer.
For example, exposure to cigarette smoke together with exposure to asbestos leads to a greatly increased risk of lung cancer.18 The risk of lung cancer from radon exposure is estimated at between 10 to 20 times greater for persons who smoke cigarettes as compared with those who have never smoked.19 The risk of cancer from consumption of alcoholic beverages is most pronounced among smokers.20 Some evidence suggests that diets deficient in micronutrients such as vitamins B2, B6, B12, and folic acid may increase susceptibility to arsenic-induced cancers.21
Environmental Exposures Linked to Cancer Risk
National and international agencies have established systems to classify agents according to the likelihood that the agent may cause cancer. This is often a difficult process because the information on an agent may be incomplete or inconclusive. Data from in vitro and in vivo laboratory studies are considered, along with human epidemiological studies, when those are available.
IARC has developed one of the most comprehensive classification schemes. In this scheme an agent is rated from Group 1 to 4 based on human and animal data.22 The table below provides a few examples of the many chemicals in each IARC category.
|
Group |
Evidence |
Examples |
|
Group 1, Carcinogenic to humans (128 agents total)* |
Sufficient human data |
Aflatoxins Benzene Chromium VI Formaldehyde Ionizing radiation PCBs (some) PFOS Radium-224 Radon-222 Silica dust Tobacco smoking Welding fumes |
|
Group 2A, Probably carcinogenic to humans (95 agents total) |
Limited human data |
Acrylamide Creosotes Human papillomavirus type 68 (HPV) Lead compounds (inorganic) Pesticides DDT, dieldrin, glyphosate, and malathion Perchloroethylene (PCE) Shift work that involves circadian disruption Styrene |
|
Group 2B, Possibly carcinogenic to humans (323 agents total) |
Limited or inadequate human data |
Carbon nanotubes, (multi-walled MWCNT-7) Chloroform Extremely low-frequency magnetic fields Gasoline Pesticides chlordane, heptachlor, mirex, naphthalene, and parathion Melamine |
|
Group 3, Not classifiable as to its carcinogenicity to humans (500 agents total) |
Not enough human or animal data |
Caffeine Diazepam Pesticides carbaryl and endrin Prednisone Toluene |
*table last updated 01/11/2024
Common Exposure Pathways
CHE’s Toxicant and Disease Database lists hundreds of specific disease-toxicant associations. Here we highlight a few common pathways of exposure that are linked to increased risk of cancer:
Air Pollution
Exhaust from cars, trucks, ships, and other vehicles, especially diesel particulates, cause up to 30 percent of air pollution-related cancers. Diesel particulate is an IARC Group 1 carcinogen with the average lifetime risk for cancer attributable as high as 1 in 1,000 people.23
Industrial combustion also creates particulate matter associated with many types of cancer. This pollution can travel through the air to nearby schools, exposing children. A 2008 investigation of almost 128,000 schools found that the majority experience toxic air pollution, and one in six schools were located within a mile of a major industrial plant.24 A study in 2022 showed that US public schools with higher proportions of impoverished and racially/ethnically marginalized students are more likely to be in areas with worse air pollution than schools with lower proportions of marginalized students. The air pollution measured was from combined traffic and industrial sources.25
Endocrine-Disrupting Chemicals (EDCs)
EDCs are found in many everyday products, including plastics, detergents, flame retardants, food, toys, cosmetics, and pesticides. These chemicals can alter the hormonal signals that control and guide much of our growth and development during infancy and early childhood, the way our organs function, and our ability to fight disease.
Exposure to EDCs is linked with many human diseases and conditions, including cancer.26 EDCs are of particular concern for children and pregnant women. Studies have shown that EDCs can have health impacts, including increasing cancer risk, at extremely low doses.
Flame Retardants
Flame retardants have been added to a range of products since the 1960s. Though many flame retardants are no longer produced, they do not easily break down, remaining in the environment for years and bioaccumulating in people and animals over time. Also, in many cases, manufacturers replaced problematic chemicals with regrettable substitutes that could cause similar health harms. Many types of flame retardants are associated with an increased risk of cancer.27
Personal Care Products
Personal care products (PCPs) such as shampoo, deodorant, and fragrance often contain chemicals of concern, such as parabens and phthalates, which can act as EDCs. These chemicals are also suspected of being one of the factors driving increases in breast cancer rates. Many of these chemicals are not disclosed as ingredients. Studies have found that women of color are often disproportionately exposed to chemicals from PCPs.28
Pesticides
There are hundreds of pesticides in many classes, each with different toxicological effects. Thus is it an oversimplification to say that pesticides as a whole cause cancer. However, exposures to certain pesticides are associated with several types of cancers. Farmers, farmworkers, and rural families are at particular risk, as these communities can face exposure to pesticides in the air and water as well as via food residues. IARC has classified many pesticides as known, probable, or possible human carcinogens (Groups 1, 2A, and 2B).29
PFAS
PFAS (per- and polyfluoroalkyl substances) are a class of more than 12,000 chemicals used in consumer products, industrial applications, and industrial firefighting foams. They are used in numerous consumer products such as food packaging, textiles, apparel, and non-stick cookware due to their stain, grease, and water resistance properties. A number of PFAS are linked to adverse health outcomes including liver and kidney damage, reproductive and developmental harm, immune system impairment, and certain cancers, such as testicular and kidney cancer.30 Many members of this large class of chemicals have not been evaluated for potential health effects.
Pharmaceutical Drugs or Treatments
IARC classifies a number of pharmaceutical drugs or treatments as Group 1 carcinogens, including:31
- Azathioprine
- Busulfan
- Chlorambucil
- Chlornaphazine
- Cyclophosphamide
- Cyclosporine (cyclosporin)
- Diethylstilbestrol
- Estrogen-progestogen oral contraceptives (combined)
- Estrogen-progestogen menopausal therapy (combined)
- Estrogen therapy, postmenopausal
- Etoposide (also in combination with cisplatin and bleomycin)
- Melphalan
- Methoxsalen (8-methoxypsoralen) plus ultraviolet A radiation
- MOPP and other combined chemotherapy including alkylating agents
- Phenacetin
- Semustine (methyl-CCNU)
- Tamoxifen
- Thiotepa
- Treosulfan
Specific Chemical Exposures
Here we highlight a few examples of specific chemical carcinogens to which large numbers of people in communities or workers in specific occupations are regularly exposed. To date, IARC has evaluated over 1,000 agents. Of those, they have determined that 128 are known to be carcinogenic to humans. Another 95 were identified as probably carcinogenic to humans and 323 are possibly carcinogenic.
However, thousands of chemicals are actively used by industry in the US and only a small fraction have been evaluated for their health impacts, including their potential carcinogenicity.
| Arsenic |
Inorganic arsenic can be found naturally in drinking water and is associated with skin, lung, bladder, and kidney cancer in both men and women and prostate cancer in men.32 |
|
Asbestos |
Asbestos, a natural mineral fiber used in many industrial materials and products, continues to cause serious human health effects. Inhalation of asbestos is the primary cause of mesothelioma, cancer of the membrane that lines several body cavities and covers some of the body’s internal organs. Some evidence indicates asbestos increases the risk of other cancers. More than 70 percent of patients with mesothelioma cancer have a history of exposure to asbestos at work.33 |
| Benzene |
Benzene is in gasoline and other transportation fuels and is widely used in the production of other products such as rubber, nylon, synthetic fiber, lubricants, glues, detergents, dyes, drugs, and pesticides; it is also used in fracking and is part of vehicle exhaust and cigarette smoke.
Liver enzymes convert benzene to more toxic metabolites, which is thought to be what causes its carcinogenicity.34 Benzene exposure increases the risk of leukemia and other blood disorders. Chronic exposure to benzene affects the bone marrow by crippling blood cell production, causing anemia. Chromosome damage can also lead to leukemia. |
| Ethylene oxide |
Ethylene oxide (EtO) is a carcinogen used as an intermediate to make other chemicals and to sterilize medical equipment and some spices. Occupational exposures occur in the workplace; residents of surrounding communities are also exposed by inhalation after intentional or unintentional releases to the environment. EtO is mutagenic. Human occupational studies show elevated cases of lymphoid cancer and also breast cancer in female workers. In animal studies, EtO causes lymphoid cancer and tumors of the brain, lung, connective tissue, uterus, and mammary gland.35 |
| Formaldehyde |
A toxicant produced by the manufacturing industry, formaldehyde can be found in building materials. It is also used as a preservative in some personal care products. Formaldehyde can cause nasopharnygeal cancer and leukemia.36 |
| Glyphosate |
Glyphosate (often referred to by the brand name Roundup) is the most commonly used broad-spectrum herbicide worldwide. It is applied to a variety of crops, especially grains and legumes, and widely used in parks, playing fields, and home landscaping and gardens. Exposure has been associated with an increased risk of non-Hodgkin lymphoma.37 It is classified as a 2A carcinogen by IARC. |
| Hexavalent chromium |
Hexavalent chromium damages DNA and can cause nasal and lung cancer. Exposure is known to occur in occupational settings (such as manufacturing, steel and alloy production, and leather tanning) and through community-wide exposure from improper disposal practices.38 |
| Perchloroethylene (PCE or Perc) |
PCE is the most common solvent used by dry cleaners in the US. The dry cleaning process exposes workers and releases significant amounts of PCE into the air. Improper storage and disposal of PCE has contaminated soil and water across the US. Breast cancer is specifically associated with PCE in drinking water.39 Studies of people exposed in the workplace have found associations with several other kinds of cancer including bladder cancer, non-Hodgkin lymphoma, and multiple myeloma. |
|
Perfluorooctanoic Acid (PFOA)
|
PFOA is the most well-studied PFAS and was recently classified by IARC as carcinogenic to humans. PFOA has been phased out of use in the US but persists in the environment. Studies have shown PFOA exposure to be associated with kidney cancer, especially in those exposed through their work or from living in communities with significant environmental contamination.40 |
| Trichloroethylene (TCE) |
TCE, used in manufacturing, is strongly associated with kidney and liver cancer and is suspected to be associated with lymphomas, leukemia, and cervical cancer. An IARC Group 1 carcinogen. Improper disposal has released TCE into water sources, and it has been detected in up to 34 percent of US drinking water.41 |
Other Contributors to Cancer
Alcohol consumption increases the risk of cancers of the breast, mouth, pharynx, larynx, esophagus and liver.42
Electromagnetic Energy/Non-Ionizing Radiation comes from wired and wireless devices. Cell phones and their towers emit radiofrequency radiation (RF) while power lines and appliances emit extremely low-frequency electromagnetic fields (ELF-EMF). The ubiquitous use of cell phones raises concern over risks posed by exposure to the EM energy emitted by these devices, and a rapidly growing body of evidence suggests that EMR/EMF may have deleterious effects on human health with prolonged exposure, including increased risk of cancer.43 IARC has classified radiofrequency electromagnetic fields as possibly carcinogenic to humans (Group 2B).44
Certain Foods are associated with some cancers. For example, processed meats (Group 1) and red meats (Group 2A) are classified as known or probable carcinogens by IARC.45 Dietary research is increasingly turning to the study of various dietary patterns rather than single nutrients or food groups and their relationship to health outcomes. Some dietary patterns are associated with increased risk of several kinds of cancer.46
Some Infectious Diseases, both viral and bacterial, are associated with an increased risk of some kinds of cancer. For example:47
- Certain strains of human papilloma viruses (HPVs) are linked to cancers of the cervix, vagina, vulva, penis, anus, and some cancers of the mouth, throat, head, and neck.
- Epstein-Barr virus (EBV) is linked to nose and throat (nasopharyngeal) cancer, lymphoma of the stomach, Hodgkin lymphoma, and Burkitt lymphoma.
- Hepatitis B virus (HBV) and hepatitis C virus (HCV) are linked to chronic liver infections, which can raise the risk of liver cancer (hepatocellular carcinoma).
- Human herpes virus Type 8 (HHV-8), also called Kaposi sarcoma herpes virus (or KSHV), is linked with a type of cancer called Kaposi sarcoma. Most people with HHV-8 do not develop Kaposi sarcoma unless they are also infected with human immunodeficiency virus (HIV), the virus that causes AIDS.
- Human T-lymphotropic virus-1 (HTLV-1) is linked with certain types of lymphocytic leukemia and non-Hodgkin lymphoma (NHL).
- Helicobacter pylori is linked to gastric cancer.48
Medical Radiation. By 2006, almost half of the typical American exposure to ionizing radiation had come from medical devices, especially from computed tomography (CT) scans. These exposures are associated with an increase in cancer risk. An adult receiving an annual CT scan for a 30-year period is projected to increase his or her overall lifetime risk of cancer mortality by almost two percent. Though it might not be significant at the individual level, it is a considerable concern across the population of patients receiving CT scans on a regular basis. Scans of young children, who are more vulnerable to radiation's effects than adults, are even more concerning.
Substantial evidence demonstrates that medical radiation is an important and controllable cause of breast cancer.49
Obesity and being overweight contribute to an increased risk of a number of different kinds of cancer.50
Radon is another source of radiation known to cause cancer (IARC Group 1 carcinogen),51 with between 15,000 and 22,000 lung cancer deaths in the United States each year related to radon.52 The main source of indoor radon is from naturally-occurring radon gas infiltration from soil into homes and other buildings in many geographical regions.
Tobacco use kills over eight million people worldwide each year, with more than six million of those deaths the result of direct tobacco use. An estimated 1.3 million deaths per year are the result of exposure to secondhand smoke among non-smokers.53
Ultraviolet Radiation, UVA and UVB, is emitted by tanning beds, sun lamps and the sun itself. Extensive evidence has demonstrated that both types of ultraviolet radiation can cause skin cancer.54
Cancer Prevention
According to the World Health Organization, up to 50% of cancer cases are preventable - and this number is likely higher if avoidable environmental drivers of cancer are fully considered.55
Cancer is a disease that affects not only individuals, but also communities. The primary cause of one person’s cancer might be very personal, such as from smoking or higher-risk genetic makeup. On the other hand, the causes of cancer and cancer patterns in a community might be very different from one place to another, and many factors that influence cancer risk are out of an individual’s control. Therefore, cancer prevention cannot be considered solely an individual responsibility.
Despite this complexity, there are many straightforward opportunities for prevention. Removing known risk factors, such as carcinogenic chemicals, will help prevent some cancers.
Policies for Prevention
Primary prevention of cancer focuses on preventing healthy people from developing cancer in the first place. This is in contrast to secondary prevention activities, such as screening to detect early-stage cancers. Primary prevention is the most cost effective and humane way to combat cancer. That’s why we support science-based policy changes that address prevention at the societal level.
Policies for prevention include stronger regulations to control the use of hazardous materials linked to cancer as well as better enforcement of those regulations. We need stronger protections for air and water quality, as well as new approaches to zoning, planning, and permitting that do not allow already burdened communities to be further contaminated by additional sources of pollution. In addition, these interventions must be developed in cooperation with the communities and workers most impacted by toxic exposures.
Policies for prevention also need to address the societal factors that strongly influence personal opportunities and choices with respect to diet and exercise, as well as workplace safety, each of which can influence cancer risk. For example, the American Institute for Cancer Research summarizes recommendations for diet and exercise that can help prevent cancer, but these opportunities are not available in all communities. Therefore, these recommendations should also be addressed with changes in public policies.
Personal Prevention Choices
In addition to diet, exercise and weight control, steps can be taken individually to reduce exposures to carcinogens in the environment. One recent study found that informed choices in personal care products (specifically avoiding the use of products containing phthalates and parabens) was likely to reduce breast cancer risk.56 Because children are particularly vulnerable to these exposures, child care providers in particular should look to reduce or remove hazardous exposures.
Here are some additional recommendations for individual actions from the President’s Cancer Panel:57
- Remove shoes before entering the home in order to keep out hazardous chemicals that could be tracked in
- Wash potentially chemically-contaminated clothing separately from other family laundry
- Filter drinking water
- Store and carry water in stainless steel, glass, or phthalate-free containers
- Microwave foods in ceramic or glass
- Purchase organic when possible and appropriate, and wash conventionally grown food before eating
- Eat free-range meat low in antibiotics and growth hormones if possible
- Avoid eating processed, charred, and well-done meats
- Consult the Consumer Product Information Database to make informed decisions when purchasing products
- Properly dispose of pharmaceuticals, household chemicals, paints, and other soil contaminants
- Turn off lights and electrical devices when not in use in order to reduce energy use and fossil fuel combustion
- Use buses, bicycles, fuel efficient cars or walk when traveling
- Avoid smoking and exposure to secondhand smoke
- Reduce electromagnetic radiation exposure by wearing a wired cell phone headset and keeping calls short
- Check home radon levels and reduce levels if needed
- Be aware of radiation exposure from medical sources
- Wear protective clothing and sunscreen while outdoors and avoid tanning beds
In addition to protecting individuals and families, some of these actions, such as purchasing organically grown food, also create economic pressure for the reduced use of cancer-causing chemicals.
CHE’s Work on Cancer
We promote cancer prevention through research, education, and effective regulation of environmental drivers of cancer. Through research, we are learning more and more about prevention. Through education, we are sharing the latest breakthroughs. And through effective regulation, we can ensure that our public policies align with the latest science.
Over the years CHE has hosted dozens of webinars highlighting scientific findings linking chemical exposures to increased cancer risk, as well as possible preventive measures — and continues to do so.
 In 2024, the organization Zero Breast Cancer (ZBC) became a project of CHE. ZBC promotes breast cancer risk reduction through translation of scientific research and evidence-based recommendations that support health and wellness at key stages of life. CHE’s partnership with ZBC is rooted in our shared commitment to translating science into action in the service of health.
In 2024, the organization Zero Breast Cancer (ZBC) became a project of CHE. ZBC promotes breast cancer risk reduction through translation of scientific research and evidence-based recommendations that support health and wellness at key stages of life. CHE’s partnership with ZBC is rooted in our shared commitment to translating science into action in the service of health.
Consensus Statements
CHE Consensus Statement on Cancer and the Environment, 2008. In partnership with the Lowell Center for Sustainable Production and the Breast Cancer Fund (now Breast Cancer Prevention Partners), CHE developed a consensus statement that lays out the scientific rationale for stronger cancer prevention and enumerates specific research and policy initiatives to prevent environmental exposures that contribute to cancer.
Consensus Statement on Breast Cancer and the Environment, 2006. CHE’s Cancer ScienceServ created this statement calling for testing of chemicals for their effects on health and the environment before they are marketed and also advocating that patient and health professional organizations add primary prevention to organizational agendas.
President’s Cancer Panel
The CHE Cancer Working Group was actively engaged in the process leading up to the President's Cancer Panel’s report on environmental drivers of cancer. Starting in September 2008, CHE partners presented evidence at public meetings convened by the panel on what was known about a variety of environmental contributors of cancer.
Margaret Kripke, PhD, co-author of the panel report, was interviewed by The New School at Commonweal on February 7, 2011. Listen to the audio recording. The video Unacceptable Risk: Dr. Margaret Kripke on Cancer and the Environment tells the story of Dr. Kripke’s research and how that research led her to rethink her assumptions about the causes of cancer and the true burden of environmentally-induced cancers. Kripke was also part of our 2022 webinar CHE Café: Cancer & the Environment, along with cancer experts Dr. Ted Schettler and Dr. Polly Hoppin.
The panel's conclusions:
- The nation needs a comprehensive policy agenda for environmental contaminants.
- Children are at special risk and should be protected.
- Continued health research in humans is needed.
- A new paradigm is needed for long-latency diseases.
- Existing regulation must be enforced and updated.
- Radiation exposure from medical sources is underappreciated.
- The medical community should consider occupational and environmental sources in diagnosis.
- Full disclosures to workers and the general public should be made regarding environmental cancer risks.
- The military should aggressively address the toxic environmental exposures it has caused.
- Safe alternatives to current chemicals are urgently needed.
The full 2010 report, Reducing Environmental Cancer Risk: What We Can Do Now, is available on the President's Cancer Panel page on the National Cancer Institute website. The report, which informs the National Cancer Program, has brought unprecedented attention to the environmental exposures that increase cancer risk.
To explore recent webinars, blogs and partner resources on cancer, see our Key Topics page.
This page was last revised in February 2024 by CHE’s Science Writer Matt Lilley, with input from Ted Schettler, MD, MPH, and editing support from CHE Director Kristin Schafer.
CHE invites our partners to submit corrections and clarifications to this page. Please include links to research to support your submissions through the comment form on our Contact page.

