Research also shows that the overall prevalence of developmental disabilities has been increasing in recent years.1 Responsible and comprehensive efforts should be undertaken to reduce or eliminate human exposure and environmental releases of toxic substances known or suspected to impair brain development.
We share here a summary of several common learning and developmental disabilities, focusing on those which are known or suspected to have environmental factors as contributors.
Prevalence
Developmental disabilities (DD) are broadly defined as severe, chronic conditions due to mental and/or physical impairments that develop by the age of 22.2 According to The Developmental Disability Assistance and Bill of Rights Act of 2000, the term developmental disabilities applies only to conditions with functional limitations in at least three of the following areas: self-care, receptive and expressive language, learning, mobility, self-direction, independent living, or economic self-sufficiency.3
As outlined by the Learning Disabilities Association of America (LDA), learning disabilities are defined as disorders in one or more basic psychological processes that may manifest as an imperfect ability in certain areas of learning, such as reading, written expression, or mathematics.4 Learning disabilities as a group are discussed in more detail under the "Specific Disorders" section below.
Comparisons across countries or across time can be extremely difficult, in part because different definitions or diagnostic criteria are used among entities.5 Tracking and recording of data are also quite variable across entities and time. Globally, there are wider variations in prevalence within than between regions.6 In the US, about one in every six children between the ages of three and 17 has one or more developmental disabilities.7
Developmental disabilities do not affect all children equally. Developmental disabilities are more prevalent among boys than girls. Prevalence rates by race and ethnicity can vary by disorder, and children with disabilities in ethnic minority groups have inequitable access to healthcare, resulting in poor health outcomes.8 Overall, children living in poverty have a higher prevalence for developmental disabilities.9
Prevalence of some developmental disabilities in children has been increasing. For example, since 2000 the prevalence of autism has increased from 1 in every 150 children to 1 in every 36 children.10 There is some debate about how much of the increase is due to changes in diagnostic definitions versus actual increases in the number of affected children.11 However, there is clear evidence that factors such as air pollution, pesticide exposure, and maternal diabetes before and during pregnancy have a role in the increased prevalence.12
Environmental Contributors
Common causes of developmental disabilities include genetic or chromosomal abnormalities, parental health and behavior (such as smoking and drinking), preterm birth, low birth weight, specific infectious diseases, and exposure of the mother or child to environmental toxicants.13
Environmental toxicants also have the ability to play a role in each of the other causal mechanisms. Research has found associations between environmental toxicants and developmental disabilities through both direct and indirect pathways,14 with the indirect associations through genetic mutation, preterm birth, and intrauterine retardation.15
Problematic chemical exposures
There is mounting evidence that exposure to air pollution, both during pregnancy and after birth, may be a contributor to impaired neurodevelopmental.16
Exposure to lead, primarily through old paint and contaminated food and drinking water, continues to be a major, preventable cause of LDD in children.
Methylmercury exposure in the womb, potentially from a mother's consumption of fish and shellfish, is known to impair neurological development.17
Exposure to organophosphate (OP) pesticides have been associated with abnormal primitive reflexes in newborns; mental and motor delays among preschoolers; and decreases in working and visual memory, processing speed, verbal comprehension, perceptual reasoning, and IQ among elementary school–age children.18
There is overwhelming evidence that multiple classes of chemicals used in plastics are contributing to problems with child brain development. These include phthalates, certain brominated flame retardants, and bisphenols.19 Project TENDR recently released a report on these concerns, along with policy recommendations.
See the “Specific Disorders” section below for additional information on learning and developmental disabilities associated with chemical exposures.
Vulnerable populations and timing of exposures
The developmental stage of an individual at the time of an exposure can make a huge difference in the outcome. An exposure that could cause severe malformations for a fetus could be harmless to an individual later in life. In general, exposures early in life (embryo, fetus, infant, and child) are more likely to cause harm to the developing and maturing brain and nervous system than exposures later in life.
Critical windows. A critical window of susceptibility is a sensitive time interval during fetal and child development when environmental exposures can interfere with physiology of cell, tissue, or organ. These windows include periods in which cells are growing rapidly, tissues are forming, and the young body is still without most protective capabilities, such as an immune system, blood brain barrier, or DNA repair system.
The Critical Windows of Development20 timeline from The Endocrine Disruption Exchange21 shows how exposures to certain chemicals can affect various anatomical systems, including the central nervous system, at different stages of prenatal development.
Preterm Birth and Impaired Fetal Growth. Children born preterm or with impaired fetal growth (low birth weight and intrauterine growth retardation) have an increased risk of many developmental disabilities.22 Prenatal chemical exposures can cause both preterm birth and impaired fetal growth. For more information regarding these toxicants please refer to the Pregnancy webpage.
Other contributors
Brain development is greatly influenced by a child's or mother's nutrition,23 experience with injury, infectious disease, and/or infection. Poverty,24 institutional environments,25 stress,26 and other adverse environments27 contribute to cognitive impairment.
Poverty increases the risk of inadequate access to education and health care, unsafe working conditions, polluted environments, and lack of access to healthy food, safe water, and sanitation. Therefore, its contribution to disability is considerable.
A brief summary of what we know of these contributors, plus any genetic contributions, is included in the discussion of each disorder and condition below.
Interacting factors
Nutrition, disease, infection, stress, and other factors can interact with chemical exposures and with each other to impact children’s developing brains. Here are a few examples:
- Children absorb more lead when they are are deficient in calcium and iron.28
- Iodine deficiency can interfere with brain development in fetuses, but women who are deficient in iodine are also more vulnerable to the effects of perchlorate. Exposure to perchlorate contributes to thyroid hormone deficiency, which limited evidence suggests in a pregnant woman can lead to intellectual disability in her child.29
- A deficiency of vitamin A increases the risk of blindness in children infected with the measles virus.30
- Animal models indicate that exposure to air pollution and stress in utero can harm cognitive abilities later in life more than either pollution or stress alone.31
- Rodent models demonstrate that lead exposure before birth might affect the stress response system in a way that harms the body and may lead to greater impulsivity.32
- In a study of children from birth to age seven, children who experienced high levels of air pollution in utero had lower IQ scores than those not exposed, but only when their mothers experienced material hardship.33
Specific Disorders Linked to Chemical Exposures
Toxicants can impact the developing brain through various mechanisms. Mercury, for example, causes cell death and alters cell migration and proliferation. Lead disrupts neurotransmission, synaptogenesis, and synaptic trimming. DDT, PCBs, polybrominated diphenyl ether flame retardants (PBDEs), phthalates, and bisphenols appear to act—at least in part—by disrupting estrogenic or thyroid hormones.34
Research on developmental neurotoxicity is limited due to an absence of systematic testing. Although more than 200 industrial chemicals have been found to be neurotoxicants in adults and 1,000 chemicals have been reported as neurotoxicants in laboratory animal studies, only a fraction of those chemicals have been assessed to determine if they contribute to neurodevelopmental disorders, even though chemicals that harm the adult brain are almost always just as or more toxic to children’s developing brains.35
Developmental disabilities associated with prenatal and childhood chemical exposures are summarized in the table below. Unless noted otherwise, information is from CHE's Toxicant and Disease Database.36 Though the database was last updated in 2016, it remains a valuable resource. We have summarized the information on toxicants in this table, supplemented from other sources as noted.
This list is not exhaustive, and many further chemicals and agents have not been studied sufficiently to determine their roles in LDDs. For definitions of the strength of evidence and more information about the database, see About the Toxicant and Disease Database. More information about specific toxicants is on the linked pages.
This list does not include non-toxicant exposures, such as electromagnetic radiation, which has been linked to neurodevelopmental problems.
|
Development Disorders Associated with Chemical Toxicants |
||
|
Disease/Disorder |
Strong Evidence37 |
Good Evidence38 |
|
Altered neurodevelopment with changes in behavior and/or attention |
|
|
|
Cerebral palsy |
|
|
|
Cognitive impairment (including learning impairments, intellectual disability, and developmental delay) |
|
|
|
Decreased coordination / dysequilibrium (ataxia) |
|
|
|
Delayed growth |
|
|
|
Fetal alcohol syndrome/fetal solvent syndrome |
|
|
|
Hearing loss (not limited to developmental loss) |
|
|
|
Minamata disease |
|
|
|
Seizures/epilepsy |
|
|
|
Visual impairment |
|
|
|
In addition to the associations above, the following toxicants are associated with unspecified neurodevelopmental effects:
Some additional associations with limited or conflicting evidence are listed in CHE's Toxicant and Disease Database. |
||
Additional information
In this section we provide additional information on select conditions and disorders with known connections to environmental exposures, listed in alphabetical order.
Ataxia (decreased coordination): Ataxia refers to clumsiness or a loss of balance and coordination that is not due to muscle weakness. This loss of coordination may be caused by a number of different medical or neurological conditions:
- Injury (head trauma, brain hemorrhage)
- Neurologic conditions
- Certain viral infections
- Exposure to toxicants (listed in the table above)
- Diet (deficiencies of certain vitamins, especially Vitamin E or Vitamin B12, or sensitivity to gluten)
- Other medical conditions affecting the nervous system (stroke, brain tumor and other cancers, diabetes, multiple sclerosis, neurosyphilis (Tabes dorsalis), immune system problems)
- Genetic disorders42
Attention Deficit/Hyperactivity Disorder (ADHD): ADHD is one of the most common neurodevelopmental disorders. ADHD runs in families, indicating that it has a strong genetic component. However, environmental factors also likely play a role.43
Autism Spectrum Disorder: One in every 100 children worldwide has an autism spectrum disorder (ASD); in the US that number is one in every 36 children.44 A study in the United Kingdom found that the recorded incidence of autism increased by 787% over 20 years. The study authors stressed that much of this increase could be due to increased reporting and application of diagnosis.45 However, other studies have increasingly shown the potential significance of environmental influences.46 There is much that is unknown about the causes of ASD. The clearest evidence involving environmental factors includes prenatal exposure to air pollution and certain pesticides.47 In addition, maternal obesity, diabetes, and immune system disorders have also been associated with an increased risk of ASD.48
Cerebral Palsy (CP): CP is the most common motor disability in children, with about one in 323 children US children diagnosed.49 The onset of CP symptoms occurs from infancy to early childhood. CP is caused by malformation of the brain or brain injury.50 Other than exposure to mercury as listed in the table above, environmental risk factors include preterm birth and lower maternal socioeconomic status.51
Down Syndrome: Down syndrome occurs when an individual has a full or partial extra copy of chromosome 21. Strong associations have been found between maternal socioeconomic status, maternal age, and chromosome 21-nondisjunction, the cause of 95% of Down syndrome cases.52 Results regarding smoking, alcohol, maternal irradiation, fertility drugs, oral contraceptives, and spermicides remain inconsistent.53
Epilepsy: Epilepsy is the fourth most common neurological condition, and epilepsy affects more than 65 million people worldwide. A traumatic injury to the brain can lead to either short-term temporary seizures shortly after the initial trauma or longer-term post-traumatic epilepsy that is caused by scarring. Military combat-associated brain injuries increase the risk of post-traumatic epilepsy.54 Toxicant exposures connected with seizures are listed in the table above. Hispanic individuals are at greater risk of epilepsy than non-Hispanics, and Blacks have higher lifetime prevalence than whites. However, active epilepsy—in which seizures are not completely controlled—is more common in whites than in Blacks. People with lower socioeconomic status have a higher rate of developing seizures and epilepsy.55 A 2005 epidemiological survey mentions epilepsy as the most frequent comorbid conditions to autism spectrum disorder.56 Strokes, brain tumors, and Alzheimer's disease can all cause epilepsy.57
Fetal Alcohol Spectrum Disorders (FASD): Defined by the CDC as conditions which occur in individuals whose mothers drank alcohol during pregnancy, FASD are marked by physical, behavioral, and learning problems. The only cause of FASD is prenatal alcohol exposure. Alcohol consumed at any stage of pregnancy—including before a woman knows she's pregnant—can cause FASD.58 Thus there is no pregnancy period in which it is safe to drink alcohol.
Unlike the other disabilities discussed on this page, FASDs are completely preventable. Despite this, within the 2018-2020 pregnant population in the US, the Behavioral Risk Factor Surveillance System (BRFSS) estimates that nearly 14 percent of pregnant women consumed alcohol. About five percent reported binge drinking in the past 30 days. As many as one percent to five percent of first-grade students in the United States might have an FASD.59 Fetal Alcohol Syndrome (FAS) is considered the most severe condition within the FASD group of conditions. The lifetime cost for one individual with FAS in 2002 was estimated at $2 million. The estimated cost to the United States for FAS alone exceeds $4 billion annually.60 While alcohol is the only causal factor of FASDs, not all alcohol consumption is the same. The quantity, frequency, and timing of consumption all impact the effect of alcohol on a developing baby.61 The impact of prenatal alcohol exposure can also be altered by environmental factors, such as nutrition, smoking, genetics, and maternal stress.62

Hearing Impairment or Loss: The World Health Organization defines hearing loss as the inability to hear as well as someone with hearing thresholds of 20 dB or better in both ears. Hearing loss may be mild, moderate, severe, or profound. It can affect one ear or both ears and leads to difficulty in hearing conversational speech or loud sounds. Hearing loss can affect a child’s ability to develop communication, language, and social skills.63 In children, nearly 60 percent of cases of hearing loss are avoidable through primary prevention.64 Hearing loss in children may result from genetic causes or complications at birth.65 Infectious disease, including rubella, cytomegalovirus, herpes, syphilis, and Zika, as well as chronic ear infections, can contribute to hearing impairments.66 Some medications can cause hearing loss, and intense sounds can also cause both temporary and permanent hearing impairment.67 Toxicant exposures contributing to hearing impairment are listed in the table above.
Intellectual Disabilities: Intellectual disabilities (IDs) are conditions that limit intelligence (such as the ability to learn, reason, and problem solve) and disrupts abilities necessary for living independently.68 Between two and three percent of American children have an ID.69 About 23% of those with ID also have epilepsy. This is more than 20 times the frequency in the general population.70
ID causal pathways include these:
- Conditions due to genetic mutations or chromosomal abnormalities, including fragile X syndrome, Rett syndrome, and Down syndrome.71
- Adverse pregnancy outcomes (such as preterm birth and inter-uterine growth retardation)72
- Some other developmental disabilities (such as cerebral palsy, autism spectrum disorders)73
In addition to directly impacting brain development, environmental toxicants (listed in the table above) can play a role in these causal pathways.
Little Things Matter: The Impact of Toxins on the Developing Brain, from the Canadian Environmental Health Atlas
Learning Disabilities: Learning disabilities (LD) are defined as disorders in one or more basic psychological processes that may manifest as an imperfect ability in certain areas of learning, such as reading, written expression, or mathematics.74 Although attention deficit/hyperactivity disorder (ADHD) is a developmental disability that can impact an individual’s ability to learn, it is not classified as a learning disability.75 Impairments in one's ability to learn due to intellectual disabilities, vision or hearing loss, or emotional disturbances are also not considered learning disabilities.76 An estimated one in 13 Americans has a learning disability.77
Some common learning disabilities include:78
- Dyslexia (reading disability)
- Dysgraphia (writing disability)
- Dyscalculia (mathematics disability)
- Apraxia of speech (motor speech disorder)
- Central auditory processing disorder
- Nonverbal learning disorder
- Visual perceptual/visual motor deficit
- Aphasia (communication disorder)
- Dyspraxia (motor and cognitive disability)
According to the Eunice Kennedy Shriver National Institute of Child Health and Human Development, current causal hypotheses include genetics, toxicant exposure (as described in the table above), and nonchemical environmental factors such as malnutrition and poor prenatal health care.79 Other nontoxicant environmental exposures associated with learning and intellectual disabilities include infectious disease (such as HiB, Haemophilus influenzae type B) and trauma.80 Microcephaly (a head that is smaller than expected when compared other of the same sex and age, usually a sign of diminished brain growth) can also lead to learning and developmental disabilities.81 Microcephaly has been of growing concern because of its causal connection to the Zika virus, which can spread via mosquitoes but also through direct transmission between humans.
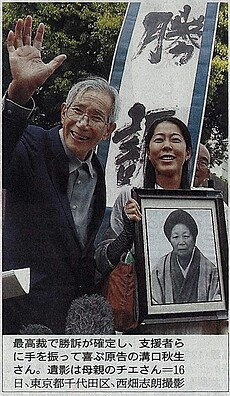
Minamata Disease: Minamata disease is named for Minamata, Japan, where the Chisso Co. Ltd. discharged waste liquid with high concentrations of methylmercury into Minamata Bay starting in 1932 and lasting until at least 1968. Minamata disease is caused by severe mercury poisoning. Symptoms include ataxia, numbness in the hands and feet, general muscle weakness, narrowing of the field of vision, and damage to hearing and speech. Severe cases involve brain damage, paralysis, incoherent speech, and delirium. A congenital form of the disease can also affect fetuses.82
Rett Syndrome: Rett syndrome affects girls almost exclusively and is characterized by normal early growth and development followed by a slowing of development, loss of purposeful use of the hands, distinctive hand movements, slowed brain and head growth, problems with walking, seizures, and intellectual disability. Apraxia—the inability to perform motor functions—is perhaps the most severely disabling feature of Rett syndrome, interfering with every body movement, including eye gaze and speech. Rett syndrome is estimated to affect one in every 10,000 female births worldwide.83 Nearly all cases of Rett syndrome are caused by a mutation in the methyl CpG binding protein 2 (MECP2) gene. Scientists have identified mutations in the CDKL5 and FOXG1 genes in individuals who have atypical or congenital Rett syndrome, but the mechanisms are still unknown. Although Rett syndrome is a genetic disorder, fewer than one percent of recorded cases are inherited or passed from one generation to the next. Most cases are spontaneous, with the mutation occurring randomly. There is some animal evidence that exposures to toxicants, including a flame retardant (BDE-47),84 may influence gene expression, especially regarding learning and memory impairment, in affected individuals.
Tic Disorders: Tourette syndrome (TS) is one type of tic disorder; the others are chronic tic disorder (motor or vocal type) and provisional tic disorder. These are distinguished by the types of tics present (motor, vocal/phonic, or both) and by the duration of the tics. Current estimates are that one out of every 160 children (0.6 percent) between the ages of five and 17 in the United States has TS.85 TS is considered a hereditary disorder, likely modified by environmental factors, but specific genes or environmental influences have not been identified.86

Visual Impairment: Young children with severe vision impairment can experience delayed motor, language, emotional, social, and cognitive development. School-age children with vision impairment can also experience lower levels of educational achievement.87 The prevalence of visual disorders is up to 10 times higher in children with developmental disabilities.88 Visual disorders are particularly increased in children born preterm, children who have suffered brain damaging events with subsequent learning difficulty, children with cerebral palsy (CP), and children who have congenital cerebral anomalies or other genetic syndromes that may predispose to ocular anomalies.89 Vitamin A deficiency is a leading cause of blindness in children worldwide.90 Toxicant exposures contributing to visual impairment are listed in the table above.
Ethical, Historical, and Social Issues
Prejudice against people with disabilities has long been an issue. Persons with disabilities, considered as a group, are more likely to experience adverse socioeconomic outcomes than persons without disabilities, including less education, worse health outcomes, lower employment, and higher rates of poverty.91 Thus adverse environments are both a cause and a consequence of some disabilities.
There is a long history of human rights violations and discrimination against those with learning and developmental disabilities. In the past, the stigma against those with developmental disabilities was so great that the medical community often encouraged families to send their children with disabilities away to institutions. These institutions were often overcrowded, understaffed, and featured inhumane conditions. The journalist Albert Deutsch described this practice of institutionalization as “ethanasia through neglect.”92
In recent decades, laws have been passed to address these issues. The Individuals with Disabilities Education Act (IDEA), first signed in 1975, ensures that children with disabilities are provided with the “least restrictive environment appropriate to their individual needs.”93 The Americans with Disabilities Act of 1990 prohibits the discrimination on the basis of disability applicable to employment, state and local government, public accommodations, commercial facilities, transportation, and telecommunications.
The Developmental Disabilities Assistance and Bill of Rights Act of 2000 seeks to ensure that individuals with developmental disabilities have access to the resources needed to “promote self-determination, independence, productivity, and integration and inclusion in all facets of community life…"94
The neurodiversity movement has sought to address the stigma around developmental disabilities. The neurodiversity movement is a self-advocacy movement largely organized by the autistic community.95 The term "neurodiversity" refers to “the diversity of human brains and minds – the infinite variation in neurocognitive functioning with our species.”96
From the concept of neurodiversity has emerged the neurodiversity paradigm. The fundamental principles of this paradigm are these:
- Neurodiversity is naturally occurring and a valuable form of human diversity;
- There is no “right” or “normal” type of brain in the same way that there is no one “right” or “normal” sex or race;
- The social dynamics around neurodiversity mirror those around other forms of human diversity.97
Along with the Autism Rights Movement (ARM), the neurodiversity movement strives to be inclusive of all neurominorities. There is quite a bit of overlap between these movements as well as ongoing debate about how to best forward these ideas. Those spearheading these efforts see these movements as part of a broader push for human rights.98
CHE’s Work on Learning and Developmental Disabilities
For years, CHE has worked with our partners to amplify emerging science on environmental factors and learning and developmental disabilities. We hosted the Learning and Developmental Disabilities Initiative in the early 2000s, leading to a joint Resolution of the Learning and Developmental Disabilities Initiative in 2003 and a national gathering at the National Institutes of Health in 2004. This meeting welcomed over 80 researchers, health care professionals, government agency representatives, philanthropists, learning and developmental disabilities advocates, and environmental health and justice leaders to explore emerging science investigating environmental impacts on neurological development and health.
CHE-LDDI hosted a dozen regional and national convenings and trainings between 2002 and 2012; explore details and proceedings here.
In addition to these gatherings, the initiative provided a forum for health professionals, scientists, researchers, community groups, government agents, and the health-affected to discuss evidence-based research regarding environmental contributors to a wide range of learning and developmental disabilities. We shared influential research articles and organized CHE Partnership calls featuring the latest science on environmental factors that can lead to neurodevelopmental problems.
CHE continues to host webinar discussions on emerging science linking chemical exposures to neurodevelopmental harms. In particular, we highlight the work of our colleagues at Project TENDR (Targeting Environmental Neurodevelopmental Risks) and promote a "better safe than sorry" precautionary approach when dealing with chemicals that may harm child brain development and contribute to learning and developmental disabilities. Both individual actions and protective public policies are needed to safeguard individuals and families.
Below are some additional core resources reflecting CHE’s work in this area.
 Mind, Disrupted: How Toxic Chemicals May Change How We Think and Who We Are, 2010
Mind, Disrupted: How Toxic Chemicals May Change How We Think and Who We Are, 2010
Scientific Consensus Statement on Environmental Agents Associated with Neurodevelopmental Disorders, 2008
Article in the Journal of Intellectual and Developmental Disability summarizing and updating these two statements: Scientific and policy statements on environmental agents associated with neurodevelopmental disorders, 2010
This page was last revised in September 2024 by CHE’s Science Writer Matt Lilley, with input from Maureen Swanson of Project TENDR (a program of The Arc), and editing support from CHE Director Kristin Schafer.
CHE invites our partners to submit corrections and clarifications to this page. Please include links to research to support your submissions through the comment form on our Contact page.