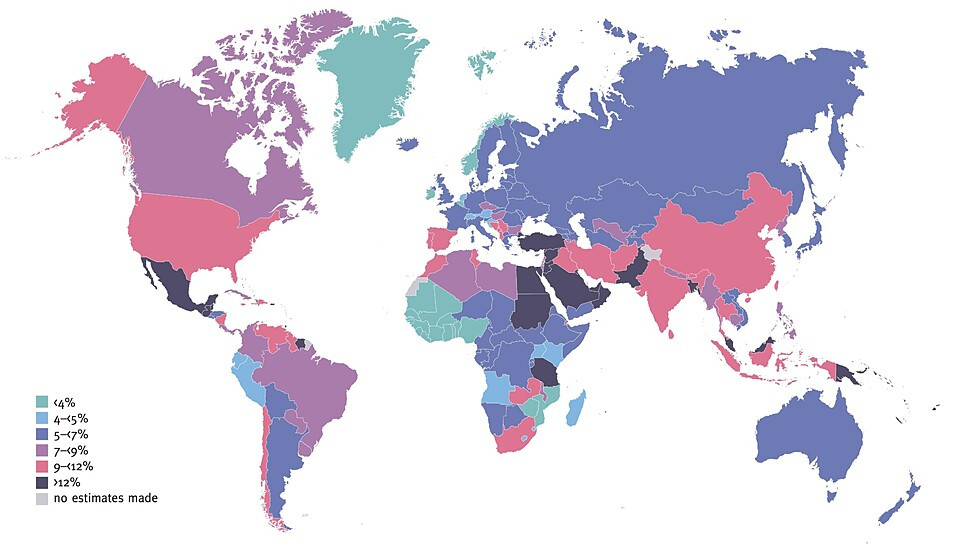
Diabetes is a large and growing global public-health concern.1 According to a 2021 report from the International Diabetes Foundation, 537 million adults are living with diabetes globally. Of those living with diabetes, 81% live in low or middle-income countries.2
Estimated Age-Adjusted Comparative Prevalence of Diabetes in Adults (20–79 years) in 2021
On this page we summarize trends in prevalence and the evidence surrounding environmental contributors to diabetes.
A Pervasive and Growing Problem
According to the most recent report from the US Centers for Disease Control and Prevention (CDC), in 2021 there were 38.4 million people living with diabetes in the United States (US).4 Among those 38.4 million, an estimated 8.7 million people are undiagnosed.
Of those aged 65 years or older in the US, 29.2 percent have diabetes, followed by 19 percent of individuals aged 45 to 64, and 4.9 percent of those aged 18 to 44.5
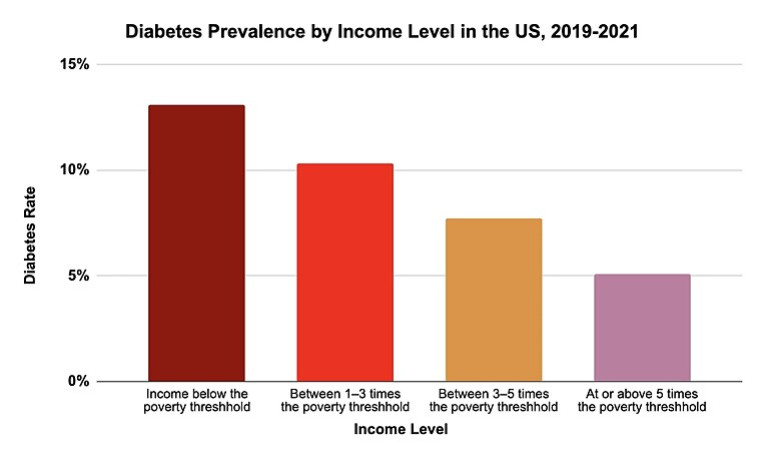
As shown below, those in the US with lower levels of income experience higher rates of diabetes.
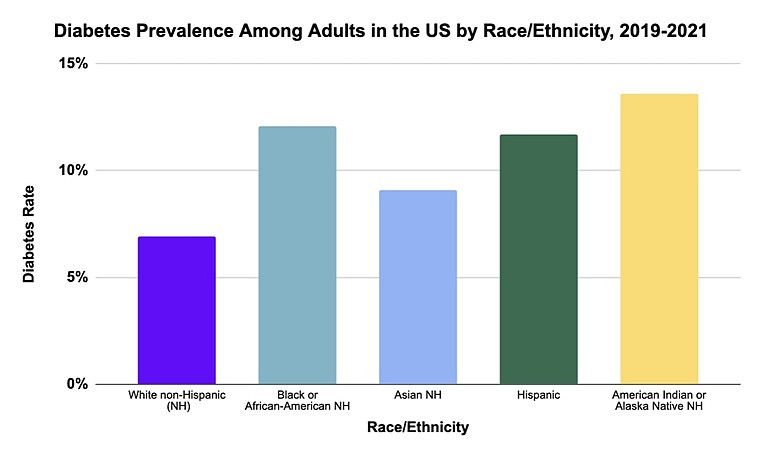
Among children, non-Hispanic whites are at highest risk for type 1 diabetes, and Native Americans are at the lowest risk. However, the reverse is true for type 2 diabetes, with Native Americans being most at risk and non-Hispanic whites being at the lowest risk.7 (See What is Diabetes? below for an explanation of the type 1 and type 2 diabetes)
Trends
The burden of diabetes, both in terms of prevalence and number of adults affected, is increasing worldwide, with the fastest rates of growth in low and middle-income countries.9
In the US, a 2014 study published in the Journal of the American Medical Association (JAMA) found the prevalence of type 1 and type 2 diabetes doubled among adults between 1990 and 2008.10 Since then, rates have continued to climb.
Trends in Age-Adjusted Prevalence of Diabetes Among Adults in the United State, 2001-2020
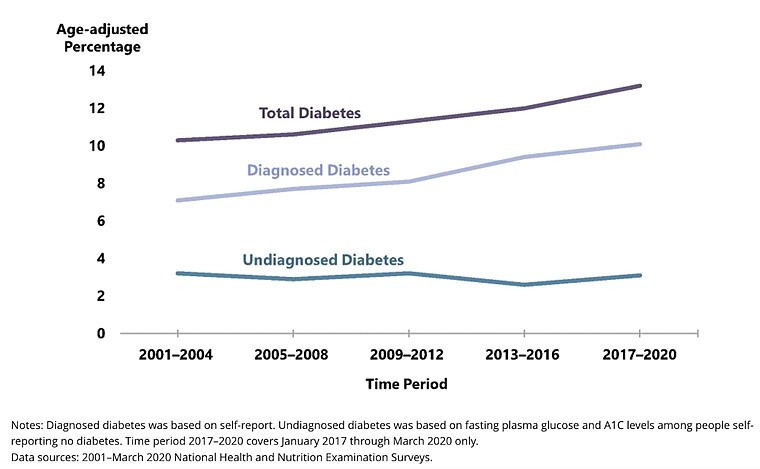
Incidence rates of both type 1 and type 2 diabetes are climbing. The incidence of type 1 has increased significantly worldwide since the 1950s.12 Recent decades have seen more of a plateau in industrialized countries, but a continuing increase in developing countries such as China.13 The highest rates of growth are among children and young people from racial and ethnic minority groups.14
What is Diabetes?
Diabetes mellitus is a class of diseases characterized by high glucose levels in the blood. The pancreas, an organ involved in digestion, releases the insulin hormone that affects the blood’s glucose content by allowing glucose to enter the body’s cells. For people who have diabetes, the glucose in the blood cannot get into the body’s cells to provide the energy needed to function.
There are three major types of diabetes, plus a condition called prediabetes.15
Type 1 diabetes is an autoimmune disease that occurs when the body does not make enough insulin. The body’s immune system malfunctions, attacking and killing the insulin-producing beta cells in the pancreas. Type 1 diabetes can develop at any age, and is often seen in childhood.16 Over 18,000 youth are diagnosed with type 1 diabetes each year in the US.17
Type 2 diabetes occurs when the body develops insulin resistance and cannot use insulin properly. Insulin resistance occurs when the body’s cells do not allow insulin to enter the cells, despite the presence of insulin in the blood. Insulin resistance can eventually lead to the pancreas's failure to keep up with insulin demands.18 Most cases occur in middle-aged and older individuals, but type 2 diabetes is now also appearing in children.19
- Overweight or low physical activity (however, 20 percent of cases occur among lean individuals, and the mechanism is not well understood)20
- A family history of diabetes
- Have had gestational diabetes
- Have prediabetes
- Being 45 or older
Gestational diabetes occurs during pregnancy. Pregnant people who are overweight or have obesity have a higher risk for developing gestational diabetes. While gestational diabetes normally resolves after birth, both the mother and baby are at increased risk of developing type 2 diabetes later in life.21
Prediabetes refers to high blood glucose levels that are not high enough to be classified as diabetes.22 Ninety-eight million people in the US have prediabetes, and eight out of ten people with prediabetes do not know they have it. Without weight loss and moderate physical activity, 15 to 30 percent of individuals with prediabetes may develop type 2 diabetes within five years.23
Related Health Problems
The major risk factors for type 2 diabetes—overnutrition, low dietary fiber, sedentary lifestyle, sleep deprivation, and depression—have been found to induce low-grade inflammation.24 Excess fat cells promote the formation of visceral adipose tissue, increasing the risk of insulin resistance and resulting in activation of pro-inflammatory antibodies, leading to a cycle of chronic inflammation.25
Those living with diabetes are at increased risk for other health problems, including:26
- Blindness/retinopathy
- Kidney failure/nephropathy
- Heart disease/cardiovascular disease
- Stroke
- Nerve damage/neuropathy
- Amputation of toes, feet, or legs
- Metabolic syndrome—a group of conditions that raise the risk of heart disease. These conditions include high blood glucose, abdominal obesity, high blood pressure, and high cholesterol/triglyceride levels27
- If type 1, then other autoimmune diseases as well (thyroid disease, celiac disease, autoimmune gastritis, and Addison's disease)28
Environmental Contributors

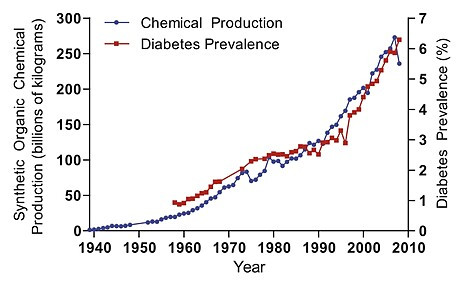
Many studies examining linkages between chemical exposure and increased diabetes risk have reported significant findings. In addition, while correlation does not mean causation, there is a striking correlation between chemical production and diabetes prevalence in the US over time.
Chemical Production and Diabetes Prevalence Over Time
The following table shows some of the major chemical exposures of concern for type 1 and type 2 diabetes. For an up-to-date summary of the studies into the risk of diabetes from these exposures, see the environmental chemicals pages on Diabetes and the Environment.
Type 1 Diabetes
|
Chemical Exposures |
Sources |
|
Traffic-related air pollution from cars, trucks, and diesel exhaust |
|
|
Contaminates drinking water |
|
|
Plastics, epoxy resins lining metal cans, thermal cash register receipts, dental sealants |
|
|
Nitrate/nitrite/N-nitroso compounds |
Nitrite can be found in processed meats; nitrate can be found in groundwater |
|
Perfluorinated compounds (PFCs), also known as perfluoroalkyl substances (PFAS) |
Used in fire-fighting foam, textiles, kitchenware, and food packaging materials |
|
Persistent organic pollutants |
Widespread environmental contaminants including PCBs, dioxins/furans, and organochlorine pesticides such as DDT |
|
Used for pest and weed control |
|
|
Rodenticide, banned in the US |
Type 2 Diabetes
|
Chemical Exposures |
Sources |
|
Traffic-related air pollution |
|
|
Contaminates drinking water
|
|
|
Plastics, epoxy resins lining metal cans, thermal cash register receipts, dental sealants |
|
|
Cadmium33 |
Used in batteries, pigments, coatings and platings, stabilizers for plastics; found in cigarette smoke
|
|
Found in the herbicide Agent Orange used during the Vietnam War, also a persistent organic pollutant |
|
|
Mercury and other metals |
|
|
PFAS |
Used in fire-fighting foam, textiles, kitchenware, and food packaging materials |
|
Phthalates |
Used as plasticizers in a variety of consumer products, like paint and cosmetics |
|
Persistent organic pollutants35 |
Widespread environmental contaminants including PCBs, dioxins/furans, and organochlorine pesticides such as DDT. |
|
Used for pest and weed control |
|
|
Radiation37 |
|
|
Selenium38 |
Soil; in some dietary supplements |
Gestational Diabetes
Growing evidence links the development of gestational diabetes to environmental chemical exposures, including phthalates, PFAS, PCBs, PBDEs, air pollution, and some metals.39
Endocrine Disrupting Chemicals
Endocrine disrupting chemicals (EDCs) are found in many everyday products, including plastics, detergents, flame retardants, food, toys, cosmetics, and pesticides. Many of the chemicals listed in the table above are EDCs. EDCs can alter the hormonal signals that control and guide much of our growth and development, the way our organs function, and our ability to fight disease. Numerous EDCs are linked to type 1 and type 2 diabetes, gestational diabetes, and obesity.
Obesity is an important risk factor for type 2 diabetes. Obesogenic EDCs are thought to stimulate adipogenesis (the process by which fat-storing cells develop and accumulate lipids). Adipogenesis is the key cellular process that leads to obesity.40 See our EDCs webpage and our page on Obesity for more details.
EDCs that are widespread in the environment, such as dioxins, pesticides, and bisphenol A (BPA), cause insulin resistance and alter beta cell function in animal models. These EDCs can accumulate in and be released from fat cells. After binding to cellular receptors and other targets, EDCs either imitate or block hormonal responses.41
Genetics & Other Factors
Genome studies have found numerous genes associated with higher or lower risks of type 1 and type 2 diabetes.42 However, genes alone cannot explain the rapidly rising rates of diabetes seen throughout the world. Some studies even suggest that genetic predisposition to type 1 diabetes is decreasing and becoming less prevalent in children.43 Diabetes is a complex, multifactorial disease; see our Gene-Environment Interaction webpage for further information on this topic.
Epigenetics
Epigenetics is a set of mechanisms that can turn particular genes or sections of chromosomes on or off.44 Environmental cues for a developing fetus or child can program persistent epigenetic modifications.45 Nutrition and exposure to certain chemicals in utero have been hypothesized to increase later risk of the offspring developing type 2 diabetes.46 Maternal malnourishment, obesity, or diabetes each may predispose the fetus to develop metabolic disease later in life.47
The EDCs described above are thought to interfere with fetal programming by affecting gene regulation and gene expression. Environmental exposures that the fetus encounters can become persistent alterations in the fetal epigenome, leading to increased risk of diabetes across multiple generations.48 The link between epigenetics and diabetes remains an active area of research.
Unhealthy Gut/Microbiome
A healthy gut is full of good bacteria that promote a healthy immune system to fight off bad bacteria and other pathogens. Broad exposure to a wealth of non-pathogenic microorganisms early in life is associated with protection against allergies, type 1 diabetes, and inflammatory bowel disease.49
Studies have found differences in gut microbiota from individuals who have diabetes and those that do not, and these differences may affect type 1 diabetes susceptibility.50 Several lines of evidence suggest that the microbiome may influence the development of type 1 diabetes, and increasing evidence suggests that microbiome-host interactions may be one environmental factor that influences type 2 diabetes risk as well as its progression.
Environmental circumstances, such as method of birth, breastfeeding, antibiotics, diet, exposure to toxics, and hygiene, can modify the microbiome.51
Lifestyle Factors
Some factors related to diabetes risk can be controlled at the individual level. Dietary choices, level of physical activity, stress, and weight have all been found to impact diabetes in various ways.
Diet: When it comes to diet early in life and type 1 diabetes in children, studies have not found unequivocal links to specific foods that increase risk.52 However, current studies are examining the protective potential of probiotics, omega-3 fatty acids, and breastfeeding.53 For type 2 diabetes, sugar-sweetened beverage consumption can increase risk.54 Human guts low in bacterial richness have been associated with higher risks of obesity and insulin resistance — both risk factors for type 2 diabetes.55 Consumption of omega-3s (primarily found in fish) have shown protective effects against type 2 diabetes.56
Physical Activity: Greater physical activity has shown to lower all-cause mortality in patients with diabetes.57
Stress: Studies show that stress is associated with type 1 diabetes development for both children and adults.58 Post-traumatic stress disorder (PTSD) and high-stress jobs have both been associated with increased risk of type 2 diabetes.59
Weight: While numerous studies indicate an association between type 1 diabetes and weight gain, other studies do not. One study found a middle ground, reporting a slight increased risk for type 1 diabetes in those with a higher BMI.60 The associations between weight gain and type 2 diabetes are well established. The Diabetes Prevention Program has found that weight reduction and intensive lifestyle interventions reduce the incidence of diabetes by 58 percent.61
Vitamin D Deficiency
Studies have found that areas with lower levels of ultraviolet B radiation (the main source of vitamin D in humans) had a higher incidence of type 1 diabetes.62 Vitamin D intake in early life is associated with a lower risk of type 1 diabetes, and maternal vitamin D intake during pregnancy may decrease the risk of type 1 diabetes in the offspring, although the evidence is not yet conclusive.63
These mechanisms—chemical exposures, lifestyle factors, vitamin D, our microbiome, and genetics—are all interconnected and act together in promoting or suppressing the incidence of diabetes.64
Costs Associated with Diabetes
According to a CDC analysis, in 2022 the direct and indirect costs of diabetes totaled $413 billion in the US.
The direct medical costs associated with diagnosed diabetes totalled $307 billion in 2022. Indirect costs of diabetes— including disability, work loss, and premature death—were calculated at $106 billion.65 According to the American Diabetes Association, one of every four health care dollars in the US is spent caring for those with diabetes.66
In addition, individuals with diabetes spend twice as much on health care as people without diabetes.67 This cost makes low-income groups even more vulnerable to the worst effects of the disease.
Impacts of societal stigma
A diabetes diagnosis oftentimes comes with stigma and blame. Individual behavior is often called into question regarding why an individual may have diabetes. These attitudes fail to take into account other contributing factors, such as environmental exposures outside of a person’s control, genetics, and social determinants of health.68
This stigma impacts many aspects of psychological well-being and may also result in sub-optimal clinical outcomes for people with diabetes.69 This can have significant impacts on both psychological and physical health.
This page was last revised in February 2024 by CHE’s Science Writer Matt Lilley, with input from Sarah Howard, MS, and editing support from CHE Director Kristin Schafer.
CHE invites our partners to submit corrections and clarifications to this page. Please include links to research to support your submissions through the comment form on our Contact page.

