Environmental health scientists look at exposures that may be harmful and determine how and why they affect human health. This approach shows us opportunities to prevent disease at both the population and individual level. CHE works with partners to share this information widely, so decision makers and individuals can make healthier decisions for themselves, their families, and their communities.
Both public policy and personal decisions can affect our environment. In environmental health, it is important to consider both the individual and the collective. Many environmental factors that influence our health cannot be controlled through individual decision making. These must be addressed at the policy level.
Environmental health often points to opportunities for primary prevention of disease – that is, preventing disease from developing, rather than diagnosing or treating it. For example, eliminating a carcinogen from our environment helps to prevent cancer, and eliminating an asthmagen from our environment helps to prevent asthma. We may never know which individuals have been protected, but at the population level, taking action helps to reduce the incidence of these and other diseases and disabilities.
Determinants of Health: The Big Picture
The chemical, biologic, physical, nutritional, built, natural, and socioeconomic environments combine to create conditions that strongly influence the health of individuals and populations. This includes social determinants of health, such as poverty and other social stressors, which are part of our environment.
We live within families, communities, ecosystems, and planetary-level conditions. The health of any part of this nested set of relationships is dependent on diverse, dynamic interactions — and can directly impact our individual health.
It is now well understood that social and environmental factors have a major influence on our health. Asthma, cardiovascular disease, diabetes, various kinds of cancer, cognitive decline, dementia, infertility, reproductive disorders, neurodevelopmental problems, and many others arise from multi-level, multifactorial circumstances.
Asthma, for example, can be caused or triggered by combinations of toxic chemical exposures, environmental contaminants, inadequate nutrition, and social stress, among other factors. These risks do not exist only at the individual level. Some, like neighborhood safety, air pollution, chemicals in consumer products, and food availability are community or societal-level factors influencing the health of everyone living there.
In a seminal paper, “Sick Individuals and Sick Populations,” epidemiologist Geoffrey Rose clarified key questions that should be asked about disease. For any individual who develops a disease, it is important to ask not only how to treat the disease, but also why the person became ill and how the disease could have been prevented. It is important to consider individual risk factors as well as risk factors that may apply to an entire community.1
Ecological models of health
Models represent how we think about, study, and try to influence outcomes amidst this complexity. Ecological models of health attempt to represent dynamic relationships within a nested hierarchy of person-family-community-ecosystem-society-planet. They feature interactions and feedback loops.
Increasingly, many medical and public health challenges are seen as systems-level problems in need of systemic interventions. Integrated, multi-dimensional, bundled interventions are most likely to be effective. Ecological models take this complexity into account and seek to identify strategic opportunities for disease prevention and treatment.

Commercial Determinants of Health
Commercial Determinants of Health (CDoH) are the private sector activities that affect people’s health. These can affect health positively or negatively. The marketing to teens of ultra-processed foods and tobacco products are two examples of CDoH that negatively impact human health.
The striking increase in non-communicable diseases over recent decades is at least partly a result of harmful CDoH. Certain corporations and industries have histories of prioritizing “wealth creation over health creation.” These organizations have been described as modern vectors of disease.
The World Health Organization (WHO) has established an initiative to address CDoH, and notes that they can often cause or exacerbate health inequities. WHO also underscores that the private sector’s influence on health policy can indirectly influence public health outcomes:
"There are multiple pathways that commercial actors influence health policy [through]. Companies commonly influence public health through lobbying and party donations. This incentivizes politicians and political parties to align decisions with commercial agendas. Further, some commercial actors work to capture branches of government in order to prevent or weaken regulation of their products and services, leading to unregulated activity, limiting their liability and bypassing the threat of litigation and pre-emption."
In contrast, companies can also choose to prioritize CDoH that improve health, such as by reformulating their goods and products to reduce harm and injury (such as when seat belts were added to cars).
Chemical exposures
More than 85,000 chemicals have been developed, distributed, and discarded into the environment over the past 50 years. The majority of them have not been tested for potential toxic effects in humans or animals.2 Whereas the toxicity of one chemical may be incompletely understood, an understanding of the effect from exposures to mixtures of chemicals is even less complete.

Some of these chemicals are commonly found in air, water, food, homes, workplaces, and communities. Air, water, food, and consumer products are all potential sources of exposure. Research has shown that household dust often contains complex mixtures of chemicals that have been released from household products.3
Occupations can be an important source of exposure. For example, firefighters can be exposed to per- and polyfluoroalkyl substances (PFAS) used in firefighting foam, and farmers and farmworkers often face pesticide exposures. Some fenceline communities, located near polluting industries, are exposed to the toxicants that those industries produce. A recent report found that plastic production facilities are almost always located near low-income communities and communities of color.4
The end of product life cycles can also cause problematic chemical exposures. People in communities living near incinerators, waste-to-energy plants, and landfills often experience higher levels of harmful chemicals in the air, water, and soil near their homes.5
Exposure assessment
Exposure assessments are used as part of a broader risk assessment process that seeks to understand the dangers from chemical or other exposures. Exposure assessments are often used to help inform environmental health policy.
Given the complexity of the routes and types of exposures, however, assessments are often difficult and incomplete, as outlined in this recent study.6 In addition, many exposures are simply unknown, due in part to lack of transparency about chemical use in products and processes. Exposure patterns and quantities also change over time, and assessments often rely on inadequate models and assumptions.
Our knowledge of what chemicals do once they are in our bodies is also incomplete. For example, much of regulatory toxicology is founded on an assumption that health effects vary predictably according to the amount of exposure, with higher doses associated with greater health effects. In reality, many chemicals have non-monotonic dose response curves, exerting significant effects at very low doses.
These and other related deficiencies lead regulators to underestimate exposures; in turn, this leads to underregulation. For more information about exposure assessment, see our blog post, “How and Why to Close the Exposure Assessment Gap,” and the 2023 webinar, “Closing the Exposure Assessment Gap: A Case Study of Phthalates.”
Windows of vulnerability
 The effects of chemicals on human health may vary, depending on timing, route, amount, and duration of exposure. Research has shown that infants and young children are particularly susceptible to the harms of chemical exposures, with windows of acute vulnerability during fetal development and early childhood.
The effects of chemicals on human health may vary, depending on timing, route, amount, and duration of exposure. Research has shown that infants and young children are particularly susceptible to the harms of chemical exposures, with windows of acute vulnerability during fetal development and early childhood.
Chemical exposures during pregnancy have been linked with lifelong consequences for maternal and child health including cardiovascular disease, diabetes, adverse infant neurodevelopment, and reproductive outcomes.7 An exposure that could be harmless to an individual later in life could cause severe malformations for a fetus.
In general, exposures early in life (embryo, fetus, infant, child, and adolescent) are more likely to cause harm than exposures at other times.
There are several reasons that children are especially vulnerable to harm from chemical exposures. Compared to adults, they breathe more air, ingest more food, and have a greater surface area relative to their body mass and volume, and their unique behaviors can bring them into more direct and prolonged contact with toxic chemicals in their environment. A child’s growth and development also makes them more susceptible to toxic chemicals (for example, lead in drinking water harming brain development).
Exposures to multiple chemicals simultaneously and other personal susceptibility factors — including genetic variability — also influence outcomes.
Gene-Environment Interactions
When disease trends are discussed in the media, possible genetic factors are often emphasized as an explanation for the incidence or prevalence of disease. However, rapidly changing rates of disease and disability cannot be attributed to genetic factors, which do not change substantially within the space of a few generations.
 It is important to understand that almost all complex chronic diseases are influenced by gene-environment interactions. Some gene variants can provide protection against the harmful effects of toxic chemicals or other hazardous exposures, while other gene variants can increase susceptibility.
It is important to understand that almost all complex chronic diseases are influenced by gene-environment interactions. Some gene variants can provide protection against the harmful effects of toxic chemicals or other hazardous exposures, while other gene variants can increase susceptibility.
The risks for common chronic diseases, such as cancer, Parkinson’s disease, and diabetes, are now known to result from the complex interactions between environmental exposures and gene variants. For example, research suggests that exposures to air pollution or pesticides in utero contribute to an increased risk of autism in those who are genetically susceptible.
Research has also shown that genetic, hormonal, and environmental factors interact with one another to influence breast cancer risk. Pesticide exposures, dietary nutrition, exercise, and nicotine may have a stronger impact on Parkinson’s risk in those who are genetically susceptible. For more information, see our resource page on Gene-Environment Interactions.
Toward a Healthier Future: Core Principles & Case Studies
Core principles can help guide us to stronger, more protective policies needed to ensure a healthier future. These include:
- Independent science. Policy should be driven by the best science available, rather than by short-term industry interests.8
- Environmental justice. Systemically marginalized communities are often the most affected by environmental harms. Promoting environmental justice is fundamental to protecting environmental health.
- Precautionary principle. “When an activity raises threats of harm to human health or the environment, precautionary measures should be taken even if some cause and effect relationships are not fully established scientifically.”9
- Sustainability. The UN defines sustainability as “meeting the needs of the present without compromising the ability of future generations to meet their own needs.”10
- Polluter pays. Requiring that polluters pay for the true costs of their activities and products can create incentives to design safer products and reduce harm.
Below are some real-world examples of these principles in action.
Tackling lead
The public health impacts of lead are now well documented, but that was not always the case. As our understanding of the hazards of lead has advanced over time, the recognized “toxic threshold” (the lowest exposure thought to be harmful) has steadily declined.11
Today, most agree that there is no safe level of exposure.12 In response to this greater understanding, there are now restrictions on the use of lead in products such as gasoline and paint.
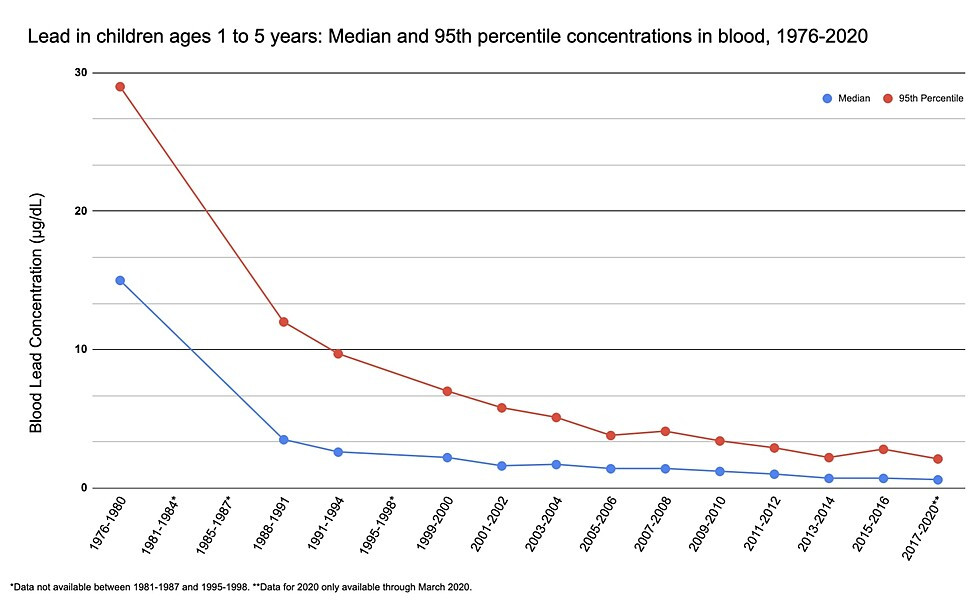
Corresponding to the public health interventions, blood lead levels in US children have declined.14
As we have seen from the drinking water crisis in Flint, Michigan, and other cities, lead still poses a serious public health problem, especially for children and others who live in lower-income urban communities. As the chart below shows, Black and lower-income children continue to be at an increased risk of lead exposure.15
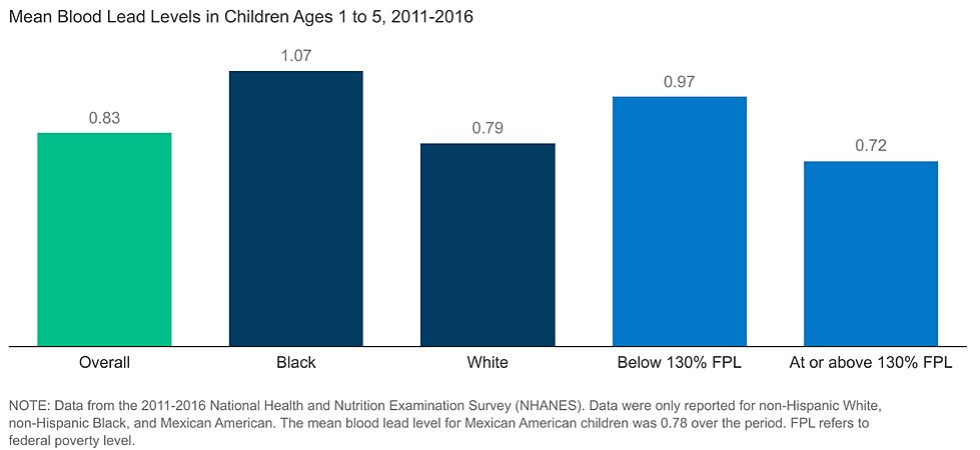
The inequitable burden of lead exposure makes clear that this is an issue of racial and environmental injustice. As a result, effective interventions need to be designed specifically with affected communities in mind, such as by carrying out more testing in schools and childcare centers in those communities.
A precautionary approach to flame retardants
Polybrominated diphenyl ethers (PBDEs) are a family of flame retardants used in many consumer products including clothing, upholstery, and electronic equipment. As a result of health concerns, many PBDEs have been phased out of use. However, these chemicals persist in the environment for years and bioaccumulate in people and animals. Once these chemicals are released into the environment, it becomes much harder to mitigate their health impacts.
In many cases, manufacturers have replaced PBDEs with less-studied chemicals whose health implications were unknown, such as organophosphate flame retardants (OPFRs) which are structurally similar to neurotoxic organophosphate pesticides. The chart below shows the estimated production of OPFRs in 2020. There is increasing evidence of their negative impact on human and ecological health.17
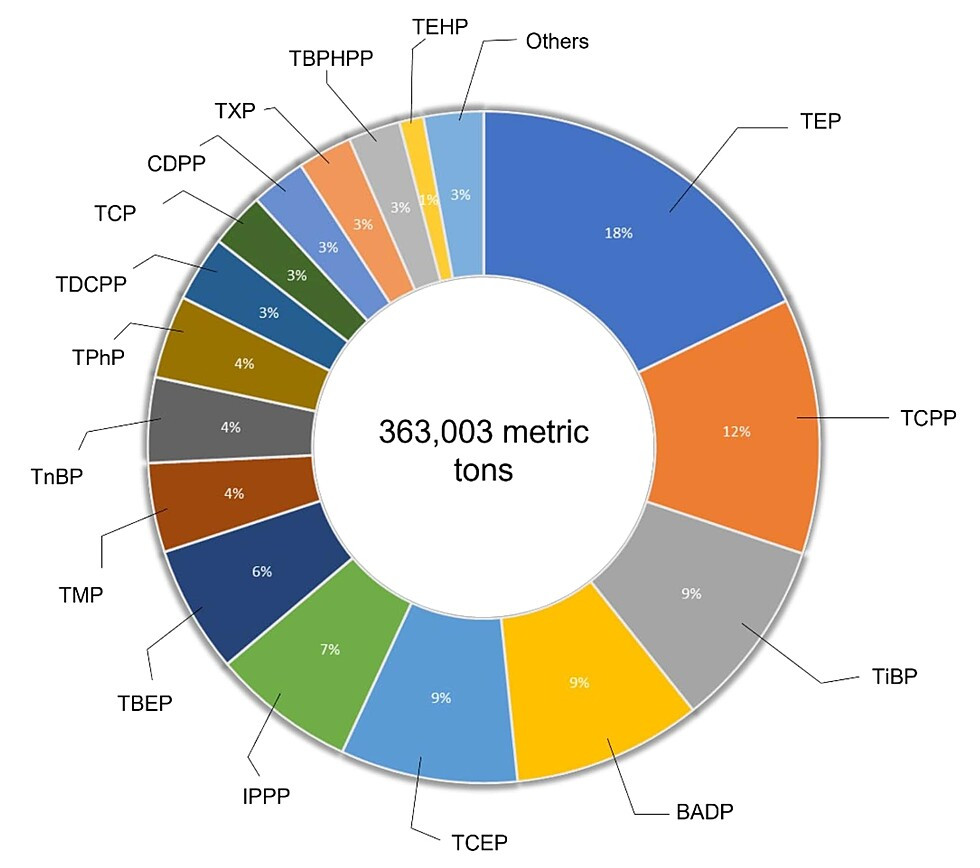
This is an example of regrettable substitution, in which one chemical known to cause health harms is replaced by an alternative that may be equally or more harmful.
By following the precautionary principle, we can stop repeating this cycle. If chemicals are tested for safety before use, we can prevent environmental damage and harm to people and communities.
Slowing unsustainable plastic production
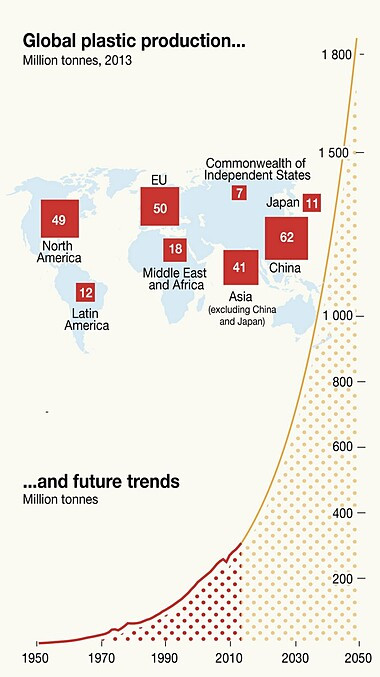
As this chart shows, plastic production is increasing rapidly.
Plastic production at these levels is unsustainable. A recent study by a group of international scientists found that "the balance of evidence is that today’s use, misuse, and production trends for synthetic chemicals (including plastics) are changing Earth system processes in unprecedented ways and are currently outstripping societies’ capacities to monitor and mitigate the problems and emerging risks.”20
Plastic production and climate change are closely intertwined. Fossil carbon from oil and gas are the main ingredients in most plastics. Greenhouse gas emissions from plastic production are on track to outpace emissions from coal-fired power plants in the US in 2030.
Each stage of the plastics lifecycle, from production to use and disposal, has adverse effects on human health. Limiting plastic production levels will, without question, protect people’s health and slow climate change.
Plastic production would not be so profitable for petrochemical companies if they paid the true price for their products. The costs of plastics in environmental and health harms are passed on to society at large and future generations. If true costs were built into single-use plastics, for example, they would be much less profitable and the petrochemical companies would be less motivated to produce at such high levels.
Following the polluter pays principle, plastic producers would pay more of the true cost of their products. Producers could be made to pay a virgin plastic fee for the plastic they make. By design, the fee would promote the use of healthier, more sustainable alternatives, and could also raise funds that would be reinvested in solutions to address the harms inherent across the plastic lifecycle.
Working together
CHE’s mission is to advance science-based policies that promote and protect the health of people, communities, and the planet.
As these examples show, we know how to arrive at healthier policies. It’s time to work together to make it happen.
This page was last revised in October 2024 by CHE’s Science Writer Matt Lilley, with input from Rachel Massey, ScD, and editing support from CHE Director Kristin Schafer.
CHE invites our partners to submit corrections and clarifications to this page. Please include links to research to support your submissions through the comment form on our Contact page.

