Pesticides are defined by the US Environmental Protection Agency (EPA) as any substance intended for preventing, destroying, repelling, or mitigating any pest.1 Although the majority of pesticide use occurs in large-scale agricultural operations, these substances are also widely used for lawn and landscape care, in-home pest control, and even direct application to the human body (e.g., lice treatments and mosquito repellents). Hundreds of pesticides are registered under the US Federal Insecticide, Fungicide, and Rodenticide Act (FIFRA).2
Types of Pesticides
Pesticides are classified by the type of pest they are targeting. While often misunderstood as referring exclusively to insecticides, the term pesticide also encompasses herbicides, fungicides, and other substances used to control pests.3
Pesticides are also categorized by chemical classes or mechanisms of action – how the chemical interacts with the body at a cellular or molecular level. The same mechanisms that make a pesticide effective against pests can also pose toxic risks to humans. Major chemical classes include organochlorines, organophosphates, carbamates, neonicotinoids, and pyrethroids, but not all major pesticides fall neatly into one of these categories.
Individual pesticides like glyphosate (an organophosphate herbicide) and atrazine (herbicide) are two examples of chemicals that have garnered significant attention due to their widespread use and human health impacts.4
Common categories of pesticides
- Insecticides kill insects
- Herbicides kill plants
- Fungicides kill fungi and mold
- Nematicides kill plant-parasitic nematodes
- Rodenticides kill rodents
- Antimicrobials kill various microorganisms, generally in preservatives, sterilizers, and disinfectants
Health Impacts
Pesticides work by interfering with biological mechanisms in pests. Because many organisms share similar biological mechanisms, the effects of pesticides often are not specific to one type of organism, and can harm organisms other than the target pest, including humans. Many pesticides are also considered endocrine disrupting chemicals (EDCs), noted for their effects on our endocrine systems, and/or persistent organic pollutants (POPs), noted for their longevity, toxicity to humans and animals, and ability to be transported around the globe through the atmosphere.
Acute exposure (poisoning)
In the United States, an average of more than 130,000 calls to poison control centers were reported from 2006 to 2010, with more than 20,000 cases treated in health care facilities annually. The Agency for Healthcare Research and Quality reported an annual average of 7,385 emergency room visits during 2006 to 2008, and 1419 annual hospitalizations during 2005 to 2009.5 Recent figures worldwide are elusive, but the WHO estimated in 1990 that there are around three million hospital admissions for pesticide poisoning each year, two million of which are as a result of deliberate ingestion, and these result in around 220,000 deaths. However, WHO also noted that "this necessarily reflects only a fraction of the real problem."6
Specific health effects and toxicity symptoms vary across both general classes of pesticides and individual pesticides within classes.
Organochlorine pesticides
Health effects and symptoms following Ingestion can include:
- Loss of sensation around the mouth
- Hypersensitivity to light, sound, and touch
- Dizziness
- Tremors
- Nausea
- Vomiting
- Nervousness
- Confusion
Organophosphate or carbamate insecticides
Common symptoms and health effects following exposure:
- Increased salivation
- Increased perspiration
- Narrowing of pupils
- Nausea
- Diarrhea
- Decrease in blood pressure
- Muscle weakness
- Fatigue
These symptoms can last up to a few days but decline as soon as acetylcholine levels return to normal in the body.
Pyrethroids
Symptoms and health effects following exposure:
- Allergic reactions
- Hyper-excitation
- Aggressiveness
- Incoordination
- Whole-body tremors
- Seizures
Other pesticides
- Acute hepatocellular injury (hepatitis)
- Acute tubular necrosis
Long-term health impacts
Establishing causality between long-term health outcomes and pesticide exposure is a challenge for researchers. These outcomes often manifest years later, and individuals are typically exposed to a complex mixture of environmental factors over time, making it difficult to disentangle the specific effect of one exposure.
We present the best available evidence below. Information in the tables below is from the Pesticide Action Network (PAN)'s Pesticides Database7 and CHE's Toxicant and Disease Database8 unless noted otherwise:
Cancer
Carcinogenicity of some common pesticides are listed below.
|
Category |
Known Carcinogens |
Probable Carcinogens |
|
Fungicides |
Maneb and nickel sulfate hexahydrate |
|
|
Herbicides and insecticides |
Arsenic and arsenic compounds |
Permethrin Organophosphates9 |
|
Wood preservatives |
Chromium VI compounds (hexavalent chromium) Creosote |
|
Reproductive and developmental effects
Pesticides linked to reproductive and developmental health impacts in summary.10
|
Categories and Common Pesticides |
Strong Evidence |
Good Evidence |
|
Fungicides Hexachlorobenzene Maneb Thiram Vinclozolin |
|
Decreased vision Fetotoxicity (miscarriage / spontaneous abortion, stillbirth) Hormonal changes Menstrual disorders (abnormal bleeding, short cycles, long cycles, irregular cycles, painful periods) |
|
Herbicides 2,4-D Alachlor Arsenic and inorganic arsenic compounds Dichlorprop Methyl bromide Propachlor |
|
Abnormal sperm Decreased coordination / dysequilibrium Low birth weight / small for gestational age / intrauterine growth retardation Seizures |
|
Insecticides Chlordecone DDT Diazinon Hexachlorobenzene Methyl bromide Nicotine Parathion |
Abnormal sperm |
Decreased coordination / dysequilibrium Decreased vision Hormonal changes Menstrual disorders Seizures |
|
Nematicides Ethylene dibromide Methyl bromide |
Abnormal sperm |
Decreased coordination / dysequilibrium Decreased vision |
|
Wood preservatives Pentachlorophenol (PCP) |
|
Other health effects
Health associations for selected pesticides; information is from CHE's Toxicant and Disease Database11 unless noted otherwise.
|
Pesticide |
Strong Evidence |
Good Evidence |
|
Aldicarb |
Immune suppression |
|
|
Carbamates |
Asthma - irritant Immune suppression |
|
|
Chlordane |
|
Immune suppression Porphyria (toxic) |
|
Chlordecone |
|
|
|
Chlorpyrifos |
|
Immune suppression Psychiatric disturbances |
|
Creosote |
Hyperkeratosis / hyperpigmentation Leukoderma (hypopigmentation) |
|
|
DDT |
Hearing loss Porphyria (toxic) Psychiatric disturbances |
|
|
Diquat |
|
|
|
Hexachlorobenzene |
Hyperkeratosis / hyperpigmentation Porphyria (toxic) |
|
|
Maneb |
|
|
|
Methyl bromide |
|
Psychiatric disturbances |
|
Nicotine |
|
Behavioral problems |
|
Paraquat |
Parkinson's disease / movement disorders |
|
|
Pentachlorophenol (PCP) |
|
Immune suppression |
|
Pyrinuron (Vacor)12 |
|
|
|
Propoxur |
|
|
|
Pyrethroids |
Pneumonitis (hypersensitivity) |
Asthma allergen, sensitizer |
|
Thimerosal |
Contact dermatitis - irritant |
|
Sensitive and vulnerable populations
As with many chemicals, fetuses and children are especially sensitive due to their continuing development. Brains, reproductive organs, and all other body systems are forming and growing, making them vulnerable to alterations. Pesticide use by parents before, during, or after pregnancy, can have long-term impacts on children, including birth defects, developmental disabilities, behavior and psychological effects, impaired reproductive function, and cancer.
Reviews have found that indoor pesticide exposure in childhood is associated with higher risk of leukemia and lymphoma,13 and occupational use of pesticides by parents is associated with a higher risk of brain tumors in children.14 An investigation in 2007 found that girls' exposure to DDT before age 14 increases their risk of breast cancer as adults five-fold. Girls exposed after age 14 did not have an increase compared to girls who were not exposed.15
Early indications of genetic susceptibility to exposures are found in studies of Parkinson's disease and cancer.16 See the Gene-Environment Interactions webpage for more information.
Environmental Justice
Pesticide exposure is a critical issue of environmental injustice, as historically marginalized communities bear a disproportionate burden of its impacts. Those who live in close proximity to pesticide production sites or agricultural areas where pesticides are heavily applied face increased exposure. There is extensive research documenting that these communities are significantly more likely to be low-income or identify as Black, Indigenous, or People of Color (BIPOC), a direct consequence of enduring systemic racism and classism.17
Additionally, the agricultural industry’s historical and current reliance on low-wage and often exploitative migrant labor, combined with the persistent lack of protections for workers in the agricultural sector – despite the inherent risks of farm labor – creates a uniquely vulnerable and underprotected workforce.18
Exposure Sources
Pesticide exposures can occur during production, use, or through contact with contaminated areas or products. They can also spread far beyond their original application site via air currents or water, leading to remote exposure. Pesticide exposure is widespread throughout the US.

For most of the U.S. population, exposure primarily occurs through pesticide residues in food and water, residential use in homes and gardens, or use in public spaces.20 Occupational exposure is another major concern, particularly for agricultural workers.
The most common routes of exposure include dermal contact (skin), inhalation, and ingestion, though exposure through the eyes is also possible. Ingesting large quantities of pesticides can result in the most harmful and serious poisonings. Pesticides can be accidently ingested through drinking from a mislabeled or reused pesticides container, which is why great care should be taken not to mix or store pesticides in food containers and to maintain and follow instructions on pesticide container labels.21
Remote exposures
 Exposures can be several steps removed from the intended use of the pesticide. For example, pesticides applied to lawns could be picked up by a pet's fur, transferred to human hands and then to food, and finally ingested.
Exposures can be several steps removed from the intended use of the pesticide. For example, pesticides applied to lawns could be picked up by a pet's fur, transferred to human hands and then to food, and finally ingested.
Pesticide residues in food and water
Low-level, often chronic pesticide ingestion occurs through residues on pesticide-treated foods. Initial studies have shown measurable, and sometimes dramatic, differences in pesticide residues in urine when a diet of pesticide-treated food sources is compared to an organic food diet.22 Due to industrial wastewater and agricultural runoff, pesticides are also detected in groundwater and streams throughout the US and globally.23
Residential exposure
Residential exposure, as classified by the EPA, refers primarily to exposure of pesticides in the home, but also includes exposures as a result of use at schools, parks, and day care centers.24 Residential exposure to pesticides occurs through both residential applications and pesticide drift.25
A recent survey shows that 75% of US households have used at least one pesticide product indoors in the previous year.26 A study of public housing complexes in Boston found pesticide residues in every surveyed home, with some homes having as many as eight different pesticides.27 Residual pesticides like chlorpyrifos can linger in household dust or on surfaces long after their application, even years after their sale has been restricted.
Occupational exposure
Workers in the agricultural sector face some of the highest risks of pesticide exposure.28 This can occur through direct handling of pesticides during application or via contaminated equipment and clothing. Occupational exposure frequently involves dermal contact and inhalation, and farmworkers often carry these pesticides home on their skin and clothing, inadvertently exposing their families.29
Reducing Exposures
The most effective way to reduce pesticide exposure is to reduce use, shifting to safer and more sustainable pest control measures.
Regulation
Measures have been put in place to restrict or eliminate use of the most harmful pesticides. In addition to the treaties and regulations linked below, many states and municipalities have put protective policies in place.
Worldwide
- Rotterdam Convention, 1998
- Stockholm Convention on Persistent Organic Pollutants, 2001
- Food and Agriculture Organization of the United Nations: The International Code of Conduct on Pesticide Management and Guidelines on Highly Hazardous Pesticides
European Union
United States
- Federal Insecticide, Fungicide, and Rodenticide Act (FIFRA)
- Federal Food, Drug and Cosmetic Act (FFDCA)
- Food Quality Protection Act
- Pesticide Registration Improvement Act of 2003 (PRIA)
- Endangered Species Act (ESA)
Personal measures
The best way to reduce pesticide exposures is to use them as little as possible. There are safer alternatives for every use of chemical pesticides, such as Integrated Pest Management (IPM) for your home and garden. In a nutshell, IPM prevents household pests naturally by removing their sources of food, water, and shelter and also their access to your home:
- Fix leaky plumbing and prevent wet spots inside and outside your home.
- Wipe up food residues on countertops.
- Seal pet food containers.
- Keep garbage contained and covered.
- Rinse recyclable containers.
- Remove woodpiles from around or inside your home.
- Repair door and window screens.
- Remove diseased plants and fallen fruit that may attract pests to your garden.
Wipe shoes on doormats and leave them at the door to avoid tracking in pesticide residues. Control dust, which can also contain pesticide residues in your home. Vacuum regularly with a HEPA filter vacuum if possible. Use damp dust rags instead of feather dusters, which stir up dust and disperse it into the air.
If you do store pesticides at home, lock them away from children's reach. Keep toxics in the original containers and follow all warning label directions.
Visit these sites for detailed information about controlling pests with methods and materials that are less toxic to children, pets and non-targeted wildlife:
- From Beyond Pesticides: ManageSafe™
- From the US EPA: Do you really need to use a pesticide?
- From Pesticide Action Network, three pages: Home, Pets, Garden
Food residues
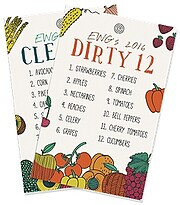 Buy organically grown produce whenever you can, especially those foods most likely to contain chemical residues. See the Environmental Working Group's annual lists of the Dirty Dozen and Clean 15 foods.
Buy organically grown produce whenever you can, especially those foods most likely to contain chemical residues. See the Environmental Working Group's annual lists of the Dirty Dozen and Clean 15 foods.
If organic produce is not available, be siure to wash fruits and vegetables. Even after washing and cooking foods however, pesticide residues may remain.
Lice treatment
Prevent head lice from becoming unwelcome guests: see Head Lice Prevention from Healthline. If you do contract lice, avoid head lice treatments that contain lindane, especially with children or anyone weighing less than 110 pounds.30
At work
 Follow all label instructions, including use of protective clothing and equipment. Measure, mix, apply, and store pesticides as directed. Ventilate areas during use if recommended. Avoid use that will contaminate water or downwind neighborhoods. Clean up spills according to the manufacturer's instructions. Wash well after handling pesticides, and especially before handling food or eating. To avoid take-home exposures, leave contaminated clothing and gear at work if possible, and wash skin and hair thoroughly before going home or having physical contact with others.
Follow all label instructions, including use of protective clothing and equipment. Measure, mix, apply, and store pesticides as directed. Ventilate areas during use if recommended. Avoid use that will contaminate water or downwind neighborhoods. Clean up spills according to the manufacturer's instructions. Wash well after handling pesticides, and especially before handling food or eating. To avoid take-home exposures, leave contaminated clothing and gear at work if possible, and wash skin and hair thoroughly before going home or having physical contact with others.
In case of an exposure, seek medical treatment promptly. If you suspect you are pregnant, take extra precaution or see if you can work away from pesticides if possible.31
In your community
 Talk to neighbors, schools, businesses, and government officials about reducing pesticide use on playgrounds, lawns, roadsides, schools, and other public areas.
Talk to neighbors, schools, businesses, and government officials about reducing pesticide use on playgrounds, lawns, roadsides, schools, and other public areas.
Case Studies: Selected Pesticides
Here we highlight two legacy pesticides that captured popular attention. They are not necessarily the most hazardous pesticides, but they achieved some notoriety and the regulatory response to the public health threats they posed provides some lessons.
Agent Orange
The US military sprayed an estimated 20 million gallons32 of Agent Orange and other herbicides on trees and vegetation during the Vietnam War. Several decades later, concerns about the health effects from these chemicals continue.33 A mixture of the herbicides 2,4-D and 2,4,5-T, which was also contaminated with dioxin (TCDD), Agent Orange has been associated with these health impacts on the Vietnamese population:
- Birth defects34 including spina bifida,35 and elevated salivary and serum cortisol and cortisone levels.36
Effects in US veterans:
- Increased incidence of diabetes, heart disease, hypertension, and chronic respiratory conditions37
- Good evidence of a link to cancer of the prostate and bladder and soft tissue sarcomas and B-cell lymphomas and also chloracne, and limited evidence of an association with Parkinson's disease; type 2 diabetes; hypertension, ischemic heart disease, and stroke; hypothyroidism; early onset peripheral neuropathy and porphyria cutanea tarda38
In 1969 the Federation of American Scientists submitted a petition to the White House with more than 5,000 signatures of renowned scientists, including 17 Nobel laureates and 129 members of the National Academy of Sciences, to end the herbicide program. In April 1970, the US government restricted use of 2,4,5-T, and therefore Agent Orange, in both Vietnam and the US. In 1971 all the remaining stocks of Agent Orange were gathered and either shipped to Johnston's Island in the South Pacific or shipped and stored at the Seabees base in Gulfport, Mississippi, from which they were destroyed by an incinerator ship in September 1977.39
DDT
Hailed as the “wonder insecticide of World War II” for protecting troops from typhus and malaria, DDT (dichlorodiphenyltrichloroethane) is an organochlorine insecticide that was widely used worldwide from the mid-1940s through the 1960s. Serious concerns about its impact on human health and the environment led the US EPA to issue a cancellation order for DDT in 1972.
Agricultural use in the US and in most countries was discontinued, but because it was widely used, because it persists in the environment without breaking down, and because it bioaccumulates in fat tissue, residues are still a concern and exposures ubiquitous.40 A 2002 review went so far as to state that “there is not a single living organism that doesn’t contain DDT."41 DDT has been detected in the Arctic, far from any production or use, and in food from all over the world.42

image from Otis Historical Archives National Museum of Health and Medicine at Creative Commons
Although DDT use is banned under the Stockholm Convention on Persistent Organic Pollutants, an exemption is granted for vector control of malaria and other insect-borne diseases, primarily in India, China, and sub-Saharan Africa.43
DDT has been associated with cancer in laboratory animals, but no clear evidence has emerged in humans.44 Based on all the available evidence, the US Department of Health and Human Services has determined that DDT is reasonably anticipated to be a human carcinogen, the International Agency for Research on Cancer (IARC) has determined that DDT is possibly carcinogenic to humans, and US EPA has determined that DDT is a probable human carcinogen.45
As an endocrine disruptor, DDT and its metabolite DDE have endocrine effects particularly during development, as demonstrated in animal tests. It can disrupt natural hormone signaling by binding to androgen receptors and blocking signals in cells, causing reproductive and developmental effects.
Studies in humans suggest that high DDT/DDE burdens may be associated with hormonally controlled endpoints such as duration of lactation, fertility, and maintenance of pregnancy. High blood levels of DDE during pregnancy have also been associated with increased odds of having preterm infants and small-for-gestational-age infants. Perinatal exposure of animals to DDT/DDE has caused alterations in the reproductive organs and infertility. In animals, DDT/DDE can produce embryotoxicity, fetotoxicity, and abnormal development of the sex organs. Adult mice administered DDT early in life showed neurobehavioral alterations when tested later in life.46
This page was last revised in December 2024 by Haleigh Cavalier, with input from Matt Lilley and editing support from CHE Director Kristin Schafer.
Some information on this page is sourced from Toxipedia.
CHE invites our partners to submit corrections and clarifications to this page. Please include links to research to support your submissions through the comment form on our Contact page.

