According to CDC guidelines, when children are found to have levels above 3.5 micrograms per decilitre (μg/dL), prompt action needs to be taken to identify and eliminate the sources of exposure to reduce the harmful health effects.1
Regulations have greatly reduced rates of lead poisoning in the United States, but we are still living with the legacy of decades-old contamination. Measures that further reduce lead exposure from legacy sources and ongoing sources, such as leaded aviation fuel, are essential to protect human health.
Around 1 in 3 children – up to approximately 800,000,000 globally – have blood lead levels at or above 5 μg/dL.2 Globally, lead poisoning accounts for an estimated 765 million IQ points lost every year.3 Lead is also hazardous to adults. The World Bank estimated that low-level lead poisoning was responsible for over 5.5 million deaths worldwide in 2019.4 Collectively, the economic cost of lead poisoning is $6 trillion every year, equivalent to 7% of global GDP.
Health Impacts
Even at very low doses, exposure to lead can impact several systems in the human body, with the nervous system the most sensitive target:5
- Cardiovascular, contributing to the onset and development of hypertension, plus coronary artery disease, peripheral vascular disease, atherosclerosis, stroke, myocardial infarction (heart attack), and arrhythmias
- Endocrine, impeding the body's ability to convert vitamin D into its hormonal form
- Nervous, this system includes the brain. Neurological effects are covered in more detail in the table below.
- Renal, including impaired kidney function and chronic kidney failure
- Reproductive, affecting sperm, fertility, time to sexual maturation, and poor pregnancy outcomes including miscarriage, stillbirth, and premature birth
Lead has the following effects on the nervous system:6
|
Children |
Adults |
|
Overt lead poisoning:
Low level lead poisoning:
|
Overt lead poisoning: Low level lead poisoning:
|
Lead storage in the body
Ingested lead circulates in the blood, but in adults 95% of lead is stored in the skeleton for years or decades until the tissue is demineralized, releasing lead back into the blood. Lead can be mobilized during these periods:7
- Pregnancy and lactation
- Periods of physiologic stress
- Chronic disease including hyperthyroidism and kidney disease
- Broken bones
- Bone infection
- Menopause
- Advanced age
Lead can be stored in a girl's or woman's body and passed to a developing fetus during pregnancy and infant during lactation many years later. A 1991 study found a higher proportion of learning disabilities among school-aged children whose mothers were poisoned by lead as children.8
Vulnerable Populations
Because lead is especially damaging to the developing brain and nervous system, the young are more sensitive to lead exposures than adults.
Fetuses, infants, and children
No safe level of lead exposure has been identified for the developing fetus or child. Lead impairs nerve cell growth and division, leading to permanent neurological damage.
Children exhibit special behaviors and characteristics that can increase their risk of lead exposure:
- More hand-to-mouth behaviors which increase the risk of ingestion of lead from paint chips, dust, and soil that adhere to hands
- Higher breathing rates than adults, leading children to intake a greater amount of lead-contaminated air
- Shorter than adults, exposing children to more lead-contaminated fumes that are close to the ground
- More lead absorption in the gut than adults, who absorb about 20 percent of ingested lead — children may absorb four or five times that amount9
Further, undernourished children are more susceptible to lead because their bodies absorb more lead if calcium or other nutrients are lacking.10
The Centers for Disease Control and Prevention (CDC) recommends that all children who are at risk for lead exposure should be tested for lead poisoning. These include children who:11
- Live or spend time in a house or building built before 1960
- Are from low-income households
- Are immigrants, refugees, or recently adopted from lower-income countries
- Live or spend time with someone who works with lead
- Live or spend time with someone who has hobbies that expose them to lead
- Live with another child who has been poisoned by lead
Children enrolled in Medicaid are required to get tested for lead at ages 12 and 24 months. They are also required to get tested if they are ages 24–72 months and have no record of ever being tested. For children not enrolled in Medicaid, CDC recommends focusing testing efforts on high-risk neighborhoods and children.
As the graph below shows, Black and lower income children in particular are at increased risk for lead exposure.
Increased Risk of Lead Exposure for Black and Lower Income Children
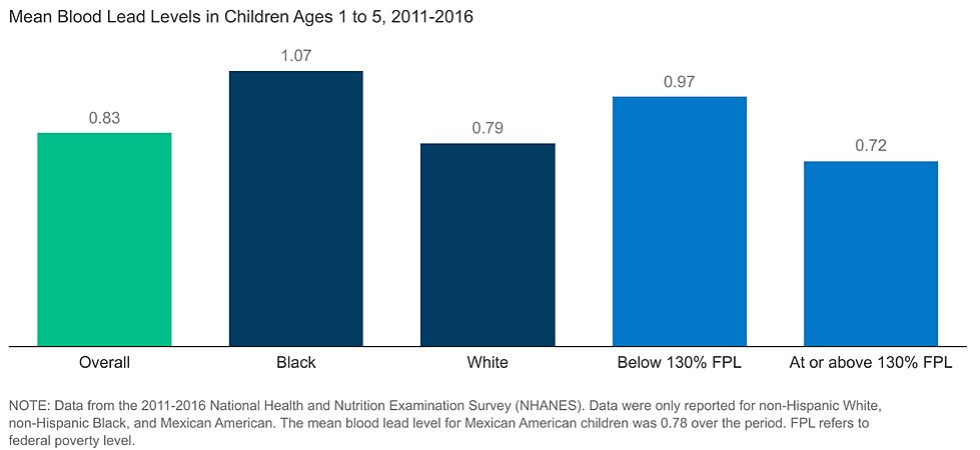
Research shows that there are direct links between structural racism, such as segregation, and environmental hazards. The disproportionate risk of lead exposure for Black children is an example of this.
Black children are significantly more likely to live in areas with older, low-income housing than white children, which partly accounts for their increased risk of lead exposure. Environmental hazards, such as proximity to industrial smelting plants or freeways, also disproportionately impact some predominantly Black neighborhoods.13

Source: US Environmental Protection Agency14
Other groups especially at risk
- Anyone who lives in a home built before lead was banned from paint (1960 in the US) — older, low-income housing is a special threat, as the leaded paint may not be maintained properly and thus creates more lead dust in the home and soil15
- Anyone who lives near or downwind from a lead manufacturing or smelting industry, past or present
- People who engage in hobbies that use lead-based materials, and those who share their homes
- Some occupations put workers at risk of lead exposure. The Occupational Safety and Health Administration (OSHA) has a standard for lead in air of 50 μg/m3, averaged over an eight-hour work-day.16 Professionals who work in jobs where they may be exposed to harmful levels of lead include:17
- Auto mechanics and repairers
- Battery manufacturers or recyclers
- Electronics recyclers
- Bridge reconstruction workers
- Construction workers
- Firing range instructors
- Gas station attendants (past exposures)
- Glass manufacturers
- Lead industry employees, including manufacturing, mining, refining, or smelting
- Plastic manufacturers
- Plumbers and pipe fitters
- Police officers
- Printers
- Rubber product manufacturers
- Shipbuilders
- Steel welders or cutters
Exposure Sources
Lead can be introduced to the body from inhaling dust particles or by ingesting lead in food, mouthing objects such as toys, or licking or sucking contaminated fingers. The most common sources of exposure for children in the US are lead-contaminated house dust, soil, water, and food.18 Other sources are also a concern.
Lead-based paint and dust
Home built before 1978 are more likely to have lead-based paint than homes built later. This paint can deteriorate and become part of the household dust. There is also danger of small children injesting paint chips. Deteriorating lead-based paint (peeling, chipping, chalking, cracking, damaged, or damp) is a hazard and needs immediate attention.19 Vinyl objects made with lead (e.g., some window blinds) can also break down and contaminate dust with lead.20
Water
Lead in water generally leaches from plumbing fixtures or lead service lines. The tragic story of water contamination in Flint, Michigan brought the problem of lead in water pipes to the world's attention.
In 2014, the city of Flint switched from Lake Huron water sourced through Detroit to a cheaper water supply, the Flint River. Even though the river water was many times more corrosive than water from Detroit, the state Department of Environmental Quality was not treating the Flint River water with an anti-corrosive agent, in violation of federal law. Corrosive water is known to leach lead from brass fixtures, lead solder, or lead service lines.
Soon after the city switched its water supply in 2014, residents began complaining that their water looked, smelled, and tasted foul. They also reported health impacts from consuming and bathing in the water. These concerns were ignored or dismissed until scientific and media investigations revealed overwhelming evidence of lead in household water at levels far above regulatory standards.21 A 2017 report by the Michigan Civil Rights Commission found that historical and systemic racism played significant roles in the Flint water crisis.22
Stories like this are neither unique nor new. Washington, DC, for example, experienced similar water contamination in the early 2000s.23
Environmental racism played a role in not only creating the Flint water crisis, but also in allowing it to continue for as long as it did.
In February 2015, a Flint resident contacted EPA regarding the extremely high levels of lead in her water. In September 2015, Dr. Mona Hanna-Attisha of Hurley Hospital found increased lead levels in children. From 2013 to 2015, the incidence of blood-lead levels above 5 μg/dL in children had doubled. In some neighborhoods, it had tripled. It was not until October 2015 that Flint switched back to the original water supply, and not until December that Flint declared a state of emergency.
It was not until November 2016 that a federal court ordered the City of Flint to ensure that all of its residents had access to safe drinking water.
The systematic exclusion of people of color from leadership roles in decisions regarding the environmental conditions that affect their lives is a key component of environmental racism. The Flint crisis persisted in part because the impacted community was systematically excluded from the decision-making process.24
Soil
Lead in soil typically comes from deteriorating house paint or nearby industrial or commercial activity, such as a gas station, firing range, or smelter.
Soil in past heavy traffic areas can still be contaminated from exhaust, due to the decades long use of lead as a gasoline additive. Lead in soil can be a problem for farmers, gardeners, and their families. See the Agriculture, Food, & Soil page for more information.
Air pollution
Lead in soils from past contamination can get resuspended into the air when that soil is disturbed. Other sources of lead emissions are ore and metals processing, particularly lead smelters, and piston-engine aircraft operating on leaded aviation gasoline.
Waste incinerators, utilities, and lead-acid battery manufacturers can also emit lead.25
EPA's National Ambient Air Quality Standards (NAAQS) air lead standard is 0.15 μg/m3 in total suspended particles as a 3-month average.26 EPA claims that "as a result of EPA's regulatory efforts, levels of lead in the air decreased by 98 percent between 1980 and 2014."27
Food
Lead in the environment can enter the food supply after being taken up by plants or ingested by animals. For instance, cereals and some vegetables grown in lead-contaminated soil can contain high levels of lead.
Lead can also enter the food supply during processing. Food cooked or served on lead-glazed ceramic or pottery dinnerware can also become contaminated.
Spices may be contaminated with lead. In some cases, suppliers of cinnamon and other spices have intentionally added lead chromate to enhance the color or increase the weight of the product.28 In some instances imported candies have been found with lead contamination. Candies with elevated lead levels appear to primarily be imported from Mexico, Malaysia, China, and India.
Some candy wrappers on imported candy may also contain lead.29
For a time, lead solder was used in cans and sometimes contaminated the food inside. Since 1995, the Food and Drug Administration has prohibited the use of lead solder in all food cans.30
Other sources
Household items

Common household and personal items that can contain lead include painted toys, keys, toy jewelry such as charm bracelets and necklaces, and vinyl objects such as toys, bibs, purses, lunch boxes, shower curtains, and mini blinds. A report released in 2024 found high lead levels in many leather and faux leather fashion accessories (purses, belts, shoes) sold at discount retailers.31
Many antique and vintage items, including furniture, ceramics, painted glasses, and jewelry can contain lead.32 Candles with lead in wicks emit lead into the air when burned. Lead in wicks was banned in the US in 2003, but older candles and candles outside the US may have lead wicks.33
Cosmetics
Some cosmetics, including some lipsticks, have discernable amounts of lead.34 Kajal (kohl), used as a cosmetic primarily by Indian families, often contains high levels of lead; prolonged application may cause excessive lead storage in the body.35 Sindoor, a red powder used on the scalp, may also be contaminated with lead.36
Hobby materials
Hobbies that involve lead-based materials can be sources of exposure as well, including:
- Home renovation, repair, remodeling, or painting (in structures built prior to 1978)
- Auto repair
- Soldering glass or metal
- Making and repairing stained glass or glazed pottery
- Molding bullets, slugs, and fishing sinkers
Traditional health remedies
Some traditional folk medicines can contain high levels of lead. For example, the following have been found to often contain lead:
- Ba-baw-san, used to treat colic pain or to pacify young children
- Daw Tway, a digestive aid
- Greta and azarcon (also known as alarcon, coral, luiga, maria luisa, or rueda), taken for an upset stomach (empacho), constipation, diarrhea, and vomiting (they are both lead-based powders)
- Ghasard, a brown powder used as a tonic for digestive issues37
Tobacco

Tobacco, its smoke, and its ash often contain lead. Both active and passive (secondhand) smoking can be sources of lead exposure.38
Artificial turf
Artificial turf playing fields, especially those made of nylon or nylon/polyethylene blend fibers, can contain potentially unhealthy levels of lead dust.39 The crumb rubber infill used with artificial turf is generally made from used vehicle tires, which can also contain lead and other metals. See our Built Environment webpage for more information.
Reducing Exposures
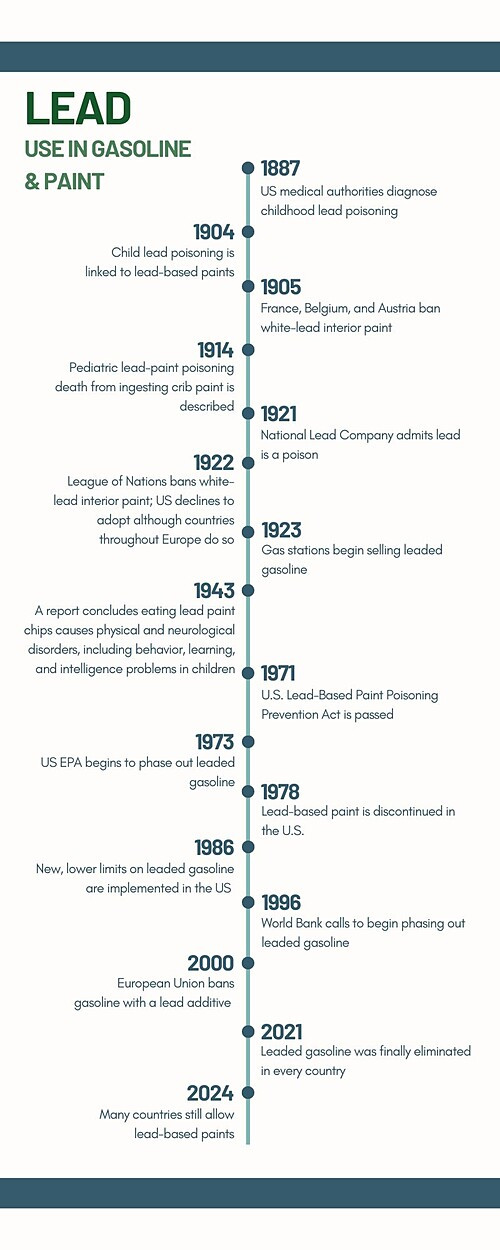
Lead has been known as a neurotoxicant for almost as long as humans have been using it.
In 1922, the League of Nations banned white-lead interior paint based on evidence of harm to children. Although several European countries adopted the ban, the US declined to do so.40 Children and their families in the US will continue to struggle with the legacy of that decision for decades.
Similarly, the addition of lead to gasoline in 1922 is said to have been one of the greatest public health failures of the 20th century.41
Regulation
Since the 1970’s, stronger regulations have greatly reduced rates of lead exposure. Lead paint was discontinued in the US in 1978. In 1973, the US EPA began phasing lead out of gasoline. Even though the Reagan Administration backpedaled on regulations starting in 1981, the primary phase-out of lead was completed in 1986.42
The graph below reflects the progress we’ve seen from better regulations.
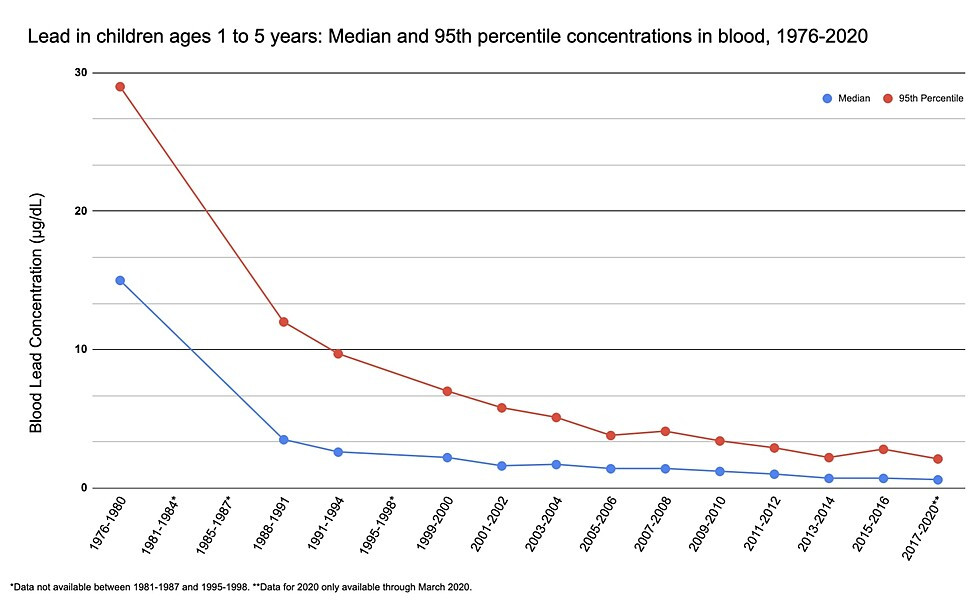
Source: US Environmental Protection Agency.43
As evidence of lead's harm has continued to accumulate, the blood lead level in children deemed acceptable by regulatory agencies has been lowered. Scientists now concur that no safe level of lead has been identified — any lead exposure is harmful to children.
In the United States, limits on lead levels have now been set for drinking water, paint, plumbing, and in occupational settings. Some states have implemented laws that are stricter than those of the federal government.
The most effective way to prevent lead poisoning is through primary prevention — removing lead hazards from the environment before anyone is exposed. In addition to being the most effective way to protect health, primary prevention is also the most cost-effective.44 Primary prevention includes things like replacing lead service lines and identifying and safely removing lead paint from homes. Community outreach and education is an important component of primary prevention.
Keeping lead out of drinking water is one area where we can do much better. EPA does have regulations for testing public drinking water systems. If more than 10 percent of tap water samples exceed 15 μg/L, then water systems are required to take additional action.45 Unfortunately, these standards are obsolete and fail to protect communities.
Experts suggest strengthening these rules by taking the following actions:46
- Set a reduced action level for water samples at 5 μg/L, which is the level recommended by Canada and the E.U
- Require water utilities to do a full inventory of their water service lines to identify all those made from lead or galvanized steel
- Require utilities to replace every lead pipe within a decade, with attention to ensuring equity in the replacement plan
- Require point-of-use water filters for those with lead service lines
- Require more robust tap water sampling
- Require public outreach to ensure that consumers at risk of lead contamination are made aware of the problem and take action to protect themselves
- Require more testing for schools and childcare centers
Globally, lead continues to be a major public health threat. In 2021, leaded gasoline was finally eliminated in every country.47 In contrast, only about half of countries have legally binding controls for lead paint. Eliminating the use of lead paint in all countries would greatly reduce exposure.
Other sources also continue to be a problem. For example, the majority of lead in use today goes into lead-acid batteries. The lead in those batteries is recyclable, but unregulated and informal lead battery recycling around the world is resulting in new lead exposures and environmental contamination.48
Personal prevention
These individual actions can help prevent exposure to lead:49
- Dust and mop frequently any spaces that children or pregnant women occupy that may contain leaded paint or other sources of lead that can contaminate dust. Use a damp rag and mop to avoid stirring dust up into the air. Promptly clean the rags and mops after use.
- In buildings built before 1960 in the US, keep paint well maintained, especially around windows and wear areas where paint is most likely to deteriorate.
- Children and pregnant women should not be present in housing built before 1978 that is undergoing renovation. They should not participate in activities that disturb old paint or in cleaning up paint debris after work is completed.
- Keep known or suspected leaded objects away from infants and children who are prone to sucking, mouthing, or chewing items.
- Avoid purchasing cosmetics that may contain lead, and keep those you have away from children.
- Avoid candy imported from Mexico made with chili powder or tamarind.50
- Use lead-free cooking and food storage containers. Some antique, handmade, and imported may contain lead in the glaze.
- Wash faces and hands of children and pregnant women often to remove lead dust, especially when living in or visiting an area where many houses have lead-based paint either inside or outside.
- Do not use the traditional health remedies that have been shown to often contain lead.
- If you know or suspect your plumbing contains lead, use water filtration (see section below); your community may also have a program to replace those lines. As an interim measure, you can flush the water from pipes before drawing water for drinking or cooking. The longer water sits in pipes, the more lead it is likely to accumulate. Hot water accumulates lead more quickly than cold water, so be sure to draw cold water for cooking and drinking. To avoid wasting water, save drawn water in a bucket for later use to refill toilet tanks.
- Shower, change, and wash clothes promptly after completing tasks where you may be exposed to lead-based products and lead dust. Do not bring lead-contaminated work clothing into a home with a child or pregnant woman.
- Check for recalls of toys and other items that have been found to contain lead. See the Consumer Product Safety Commission website.
Water filtration
Boiling water does not remove lead hazards and may even increase the concentration of lead in the water. However, a variety of methods are available for reducing lead in tap water:51
- Reverse osmosis filters
- Distillers
- Undersink filters
- Countertop filters
- Faucet filters
These devices come in a variety of designs, prices, and operating costs. Care should be taken to ensure that a filter is effective at removing lead before purchase, as not all filters are designed to remove lead.
Calcium intake
Women who may have experienced lead exposures at any time in their lives should take extra care when pregnant or lactating (breastfeeding) to follow the recommendations for dietary calcium intake. A lack of calcium in a mother's body may accelerate demineralization of her bones and teeth to supply calcium to her fetus or to her milk. If she has lead stored in her bones, demineralizations will mobilize lead into her blood.
Lead paint and remodeling considerations
Homes in the US may still have lead paint present, both inside and outside. The release of leaded paint into dust is a particular concern during remodeling. Great care must be taken to avoid introducing paint dust into the air when scraping, sanding, or cleaning deteriorating lead paint.
Even very tiny amounts of lead paint are hazardous. One chip of leaded paint the diameter of a pencil eraser ingested by a child can raise the blood lead level to a critical amount requiring immediate treatment, and the level may stay elevated for several years. Lead paint particles in dust that is inhaled can be absorbed at higher levels than ingested lead.52
EPA's Renovation, Repair and Painting Program requires certification for any firms performing renovation, repair, and painting projects that disturb lead-based paint in homes, child care facilities, and pre-schools built before 1978. EPA also publishes guidelines for do-it-yourself remodelers.
For more of our work on this topic, click here to explore webinar recordings related to lead and environmental health.
This page was last revised in June 2024 by CHE’s Science Writer Matt Lilley, with input from Dr. Bruce Lanphear and Dr. David Bellinger, and editing support from CHE Director Kristin Schafer.
CHE invites our partners to submit corrections and clarifications to this page. Please include links to research to support your submissions through the comment form on our Contact page.
Some information on this page is sourced from Toxipedia.