Hormones act like messengers, traveling through the body to deliver instructions. The endocrine system controls the body’s hormones, which maintain countless bodily functions. Chemicals that disrupt the endocrine system can produce adverse developmental, reproductive, neurological, and immune effects. Because hormones regulate growth and development, fetuses, infants, children, and adolescents face particular dangers from endocrine disruption.1
Many different chemicals and classes of chemicals can cause endocrine disruption. EDCs are a particular concern for the following reasons:
- They are everywhere. EDCs are found in many everyday products, including plastics, food, toys, and personal care products.
- They can cause harm at very low doses. EDCs can have health impacts at doses below those captured by traditional risk assessment methods.
- They can have delayed effects. The health impacts from EDCs can take many years to manifest, even potentially across generations.
Health Impacts
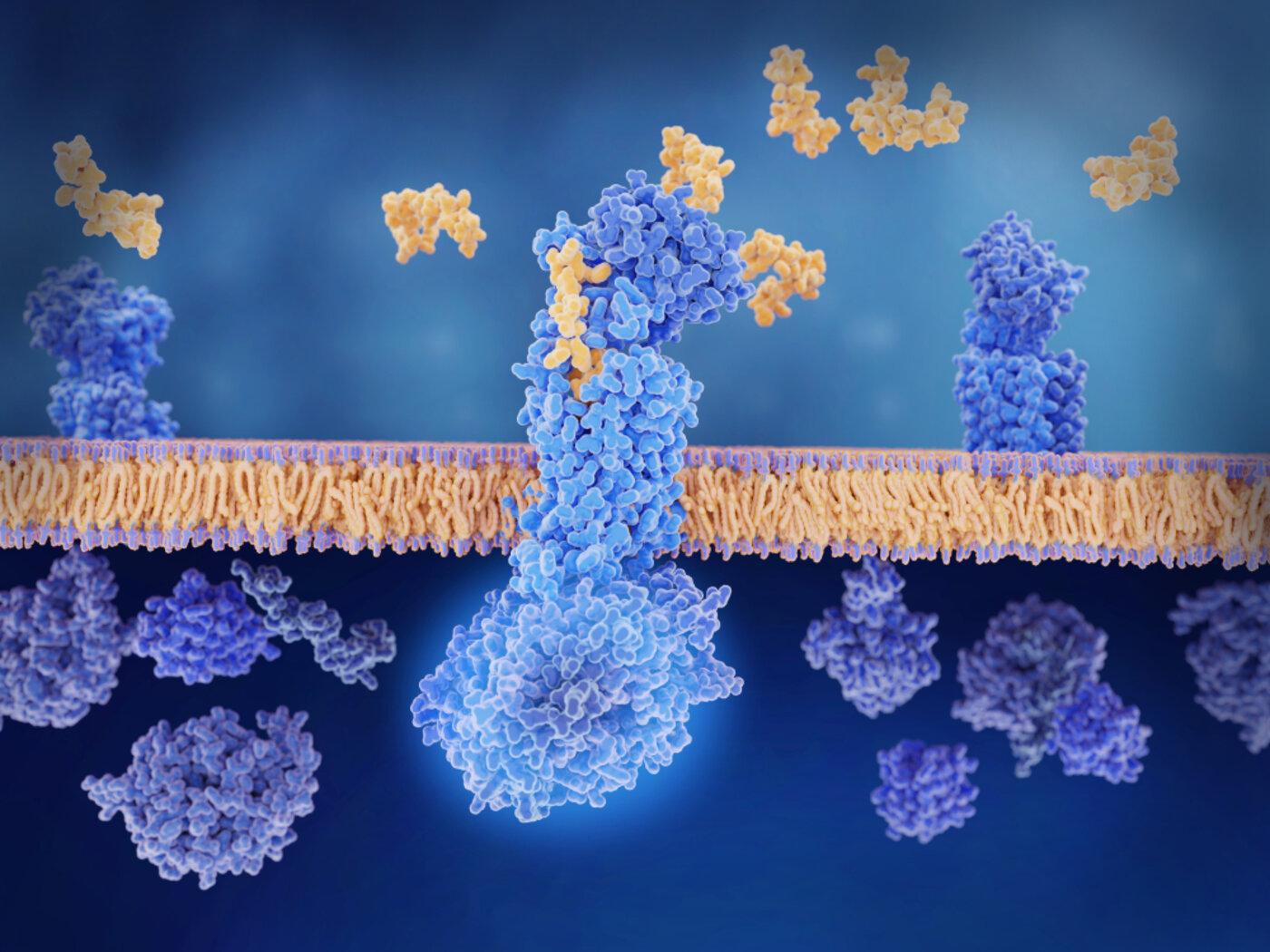
EDCs can exert their effects through a number of mechanisms:
- They may mimic the biological activity of a hormone by binding to a cellular receptor, leading to an unwarranted response by initiating the cell's normal response to a naturally occurring hormone at the wrong time or to an excessive extent (agonistic effect).
- They may bind to the receptor but not activate it. Instead, the presence of the chemical on the receptor will prevent binding of the natural hormone (antagonistic effect).
- They may bind to transport proteins in the blood, thus altering the amounts of natural hormones in circulation.
- They may interfere with the metabolic processes in the body, affecting the synthesis or breakdown rates of the natural hormones.2
Endocrine disturbances can result in cancer, IQ loss and intellectual disabilities, autism, ADHD, obesity,3 adult diabetes, disruption of thyroid and ovary function, and lowered fertility. Exposures to endocrine disruptors during pregnancy and during infancy can produce life-long effects.4
Characteristics of EDCs
Over 1,000 manufactured chemicals are known to act as EDCs. Tens of thousands of others have never been tested for endocrine disruption.5 6
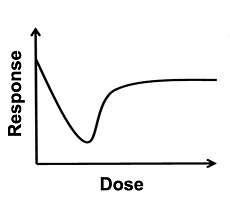
Multiple studies have shown that EDCs have the potential to produce non-monotonic responses.7 A non-monotonic response is one where there is a nonlinear relationship between dose and effect.
Traditional toxicology often uses a model in which low-dose exposures are extrapolated from data about higher-dose exposures. This approach assumes a linear dose-response curve, and fails to account for non-monotonic dose-response relationships. Thus, traditional approaches to toxicology can completely miss some of the most important ways in which endocrine disruptors affect biological systems.
Researchers have developed a framework to identify the key characteristics of EDCs. Chemicals with one or more of these key characteristics can be considered suspected EDCs and evaluated further.
Ten key characteristics of EDCS have been identified:
- Interacts with or activates hormone receptors
- Antagonizes hormone receptors
- Alters hormone receptor expression
- Alters signal transduction in hormone-responsive cells
- Induces epigenetic modifications in hormone-producing or hormone-responsive cells
- Alters hormone synthesis
- Alters hormone transport across cell membranes
- Alters hormone distribution or circulating levels of hormones
- Alters hormone metabolism or clearance
- Alters the fate of hormone-producing or hormone-responsive cells
For more information, read the consensus on the key characteristics of endocrine-disrupting chemicals as a basis for hazard identification.8
Some EDCs & specific health outcomes
Out of the thousands of manufactured chemicals that are known or suspected endocrine disruptors, here are just two examples. These illustrate the health harms of EDC exposure and the problem with delaying precautionary policy changes until long after the harms become apparent.
Diethylstilbestrol (DES) is a synthetic estrogen created in 1938; from the 1940s through the 1970s it was added to livestock feed to enhance muscle growth9 and prescribed to women with the goal of preventing miscarriages.10 The medical community discontinued its use after a 1971 article in the New England Journal of Medicine reported an association between fetal exposure during the first trimester of pregnancy and a rare cancer (clear-cell adenocarcinoma) that manifested decades later in adolescents and young women who were exposed in utero.
DES daughters and sons experience a variety of diseases and disorders linked to their prenatal exposure to DES. More research has been conducted on DES daughters than on DES sons. DES daughters experience higher rates of the following diseases and disorders:11
|
Increased Risk of Disease to Daughters from Prenatal DES Exposure12 |
|
|
Preterm delivery |
4.7 times higher |
|
Clear-cell adenocarcinoma |
40 times higher |
|
Neonatal death |
8 times higher |
|
Loss in second trimester pregnancy |
3.8 times higher |
|
Ectopic pregnancy |
3.7 times higher |
|
Stillbirth |
2.4 times higher |
|
Infertility |
2.4 times higher |
|
Early menopause |
2.4 times higher |
|
Breast cancer |
1.8 times higher |
DES sons have an increased risk for non-cancerous epididymal cysts (growths on the testicles).13 Although DES was discontinued as a prescribed medication in 1971, it was used as a feed additive in cattle until 1979.14
Atrazine is one of the most widely used herbicides in the United States. Atrazine has been linked to the following health effects:15
- Abnormal birth weight
- Birth defects, such as gastroschisis and choanal atresia
- Breast Cancer
- Infertility
- Irregular menstrual cycles
- Neurotoxicity
- Slowed metabolism
A study in 2002 showed that atrazine has extreme reproductive effects on frogs. Later studies have had similar findings, including one from 2010:16
“Ten percent of the exposed genetic males developed into functional females that copulated with unexposed males and produced viable eggs. Atrazine-exposed males suffered from depressed testosterone, decreased breeding gland size, demasculinized/feminized laryngeal development, suppressed mating behavior, reduced spermatogenesis, and decreased fertility.”
In 2020, atrazine was reapproved by EPA for use in the United States. This approval was granted despite EPA finding that the continued use of atrazine would likely harm over 1,000 endangered or threatened plants and animals.17 In contrast, the European Union banned the use of atrazine in 2003.
Disease & Economic Burden of EDCs
In 2015, an expert panel in the European Union came to consensus on the disease and economic burden resulting from EDC exposure. They were able to assess the probability of causation for EDC exposures and disease outcomes and then quantify the cost to society for the resulting disease burden. Expert panels achieved consensus at least for probable (>20%) EDC causation for IQ loss and intellectual disabilities, autism, ADHD, childhood and adult obesity, adult diabetes, male genital tract malformations, male infertility, and disorders associated with testosterone signaling.
They estimated these disease endpoints cost the EU €157 billion, 1.23% of the gross domestic product (GDP), equivalent to $209 billion US dollars, annually.18
In 2016, a similar panel of experts estimated that the disease costs of EDCs in the United States were much higher, at $340 billion (2.33% of GDP). The difference in the health effects and costs between the United States and the European Union are the result of regulatory differences, which shows the importance of effective public policy.
The health costs in the United States from flame retardants, for example, are much higher than in the European Union. This is the result of higher use of PBDE flame retardants in the United States.19 Most PBDEs have now been banned or phased out of production, but, due to their extensive prior use and chemical persistence, they remain in the environment.
Plastic chemicals are a major source of EDCs. EDCs that are used in or produced by plastics include bisphenols, phthalates, PFAS, flame retardants, and dioxins. An analysis from 2024 estimated that the plastic-attributable disease burden from EDCs in the United States was $249 billion.20
Exposure Sources
Below are examples of EDCs, some of which are discussed in more detail on their respective webpages on this site:
- Bisphenols, such as BPA or BPS, used in polycarbonate plastics and epoxy resins, among other applications. Bisphenols are commonly used on thermal receipt paper and in the linings of food containers.
- Dioxins, unwanted byproducts from various industrial processes, including the burning of plastics.
- Flame Retardants, both older flame retardants that were phased out because of health concerns and newer flame retardants that likely have similar health impacts. Flame retardants are commonly added to upholstered furniture, baby products, and car seats.
- Pesticides, used both in agriculture and in homes and gardens.
- Parabens, a group of chemicals widely used as artificial preservatives in cosmetic and body care products.
- PFAS, a class of chemicals used around the globe in a wide array of products such as non-stick cooking pans, cosmetics, paper food packaging, and clothing.
- Phthalates, a group of chemicals commonly used in plastics.
- Artificial fragrances, which often contain phthalates, parabens, and synthetic musks. These fragrances are used in many personal care and cleaning products.
- Triclosan, an antimicrobial agent found in many products, including disinfectants.
EDC exposure is an environmental justice issue in several ways. For example, studies have shown that women of color, particularly Black women, are disproportionately exposed to consumer product chemicals, including parabens and phthalates.21 The community-based Taking Stock study has found that even when women make efforts to avoid chemicals like phthalates in their personal care products, they still have biomarkers of exposure. In addition, exposures from industrial processes disproportionately impact communities of color and communities and workers of color are disproportionately exposed to agricultural pesticides.
Reducing Exposures
Regulation
A 2023 review identified several science-based policy actions that could be taken to reduce exposures to EDCs, including the following:22
- Testing: Enforce existing mandates to test chemicals for endocrine-disrupting properties.
- Screening: Make the screening of chemicals for endocrine disruption mandatory.
- Restrictions: Restrict the use of EDCs, especially in food and food contact materials.
- Coordination: Coordinate regulations between government agencies, so that if one agency restricts an EDC, the restriction will apply to other regulatory agencies as well.
- No-threshold approach: Because there are no known safe levels of exposure to EDCs, regulations and enforcement should apply a no-threshold approach.
- Hazard-based decision-making: Use hazard-based decision-making, which regulates chemicals based on their inherent properties and eliminates the need for time-consuming and often flawed exposure assessments.
- Precautionary principle: Follow the precautionary principle; new chemicals should be proven safe before they are put into use.
- Regulate by class: Regulate classes of chemicals, rather than individually.
- Account for mixtures and cumulative exposures: Require that health assessments account for real-world mixture and cumulative exposures.
The Environmental Protection Agency (EPA) is mandated to test pesticides for endocrine disruption, but has actually tested very few pesticides. The Food and Drug Administration (FDA) is responsible for regulating food ingredients and contact materials, but has no requirement for EDC testing.23
Personal Prevention
Policy change is needed at the state, national, and international level to protect people from harmful exposures. But in the absence of adequate regulatory protections, there are some actions you can take to reduce your own exposure to EDCs. A recent article from Environmental Health News explained the following steps individuals can take to reduce their risk:24
- Choose unscented products. Cosmetics, laundry detergents, cleaning products, diapers, garbage bags, and candles often have added scents that are hazardous to health.
- Avoid handling receipts. If you need to handle receipts at work, wear gloves if possible. Wash your hands with water, not hand sanitizer, after handling receipts.
- Never microwave or heat food in plastic, including plastic packaging labeled “microwave safe.”
- Avoid Teflon and other nonstick cookware. Use cast iron, stainless steel, glass, and food-safe ceramic.
- Minimize exposure to pesticides by choosing organic food when possible and avoiding the use of toxic lawn and garden chemicals.
- Wash new items before use. Avoid clothing labeled as stain or grease resistant.
- Use nontoxic cleaning products such as white vinegar, baking soda, and Castile soap.
- Dust and vacuum frequently. Household dust — contaminated with microplastic fibers, floor sealants, and flame retardants — is a major source of exposure to endocrine disruptors.
If you have the resources to do so, these additional steps can also help:
- Buy clothing, towels, and other textiles made from natural, untreated fibers such as cotton, wool, hemp, and linen.
- Replace foam mattresses and upholstered furniture with items made from wool, cotton, and natural latex.
- Buy an air filter to reduce air pollutants and minimize dust.
- Install a water filter. A two-stage or reverse osmosis water filter is possibly the most effective form of water filtration, but an activated carbon filter is also useful.
The field of endocrine disruption was founded by Theo Colborn, who co-authored the groundbreaking 1996 book Our Stolen Future: Are We Threatening our Fertility, Intelligence, and Survival? A Scientific Detective Story, along with Dianne Dumanoski and Pete Myers.25 For more on the history of this field, listen to the recordings of our calls on the 10th and 20th anniversaries of Our Stolen Future’s publication.
To explore recent webinars, blogs and partner resources on EDCs, see our Key Topics page.
This page was last revised in December 2024 by CHE’s Science Writer Matt Lilley with input from Dr. Rachel Massey and Sarah Howard, and editing support from CHE Director Kristin Schafer.
Some information on this page is sourced from Toxipedia.
CHE invites our partners to submit corrections and clarifications to this page. Please include links to research to support your submissions through the comment form on our Contact page.